Radiation Oncology/Cervix/Brachytherapy
< Radiation Oncology < Cervix|
Front Page: Radiation Oncology | RTOG Trials | Randomized Trials | |
|
Cervix: Main Page | Overview | Micro-invasive | Early Stage Non-Bulky | Early Stage Bulky | Locally Advanced | Brachytherapy | Cervix Randomized | GOG Trials | RTOG Cervix | |
Intracavitary brachytherapy
Three systems:
- Paris system
- Stockholm system
- Manchester system
- Madison system (HDR)
Manchester system
- Point A dose definitions:
- Allegedly, Point A corresponds to the paracervical triangle in the medial edge of the broad ligament where the uterine vessels cross the ureter
- Original definition: draw a line connecting the superior aspects of the vaginal ovoids and measuring 2 cm superior along the tandem and then 2 cm perpendicular to this. (weakness: failure of localization radiographs to show the surface of the ovoids' caps)
- Revised definition #1: 2 cm above the external cervical os and 2 cm lateral to midline
- Revised definition #2 (1953, Tod & Meredith): 2 cm above the distal end of the lowest source in the tandem and 2 cm lateral to the tandem
- Common variation: use flange at cervical os
- Point B - 5 cm lateral from the midline at the same level as Point A
The Manchester applicators consisted of a rubber tandem and two ellipsoid "ovoids" with diameters 2, 2.5, and 3 cm. No shielding in ovoids, so needed generous packing anteriorly and posteriorly. Used radium. Used 17.5, 20, and 22.5 mg Ra for the small, medium, and large ovoids, respectively.
Designed such that:
- Point A dose rate was approximately 0.53 Gy/hr for all allowed applicator loadings
- Vaginal contribution to Point A was limited to 40% of the total dose
- The rectal dose should be 80% or less of the Point A dose
Prescribed 80 Gy to point A in two applications, total of 144 hours, in the absence of external beam.
Weakness: wide variation in Point A in respect to the ovoids. Point A often occurs in a high-gradient region of the isodose distribution. Therefore, minor differences in position can result in large differences in dose.
References:
- No PMID - M. Tod and W. Meredith, A dosage system for use in the treatment of cancer of the uterine cervix. Br J Radiol 11 (1938), pp. 809–824.
- Revised (1953) - PMID 13042092 — "M. Tod and W. Meredith, Treatment of cancer of the cervix uteri—a revised “Manchester method.”. Br J Radiol 26 (1953), pp. 252–257.
Fletcher applicator
Derives from the Manchester system. Added internal shielding in the colpostats. Afterloading ability. Colpostat has 2 cm diameter that can be increased to 2.5 or 3 cm by the addition of plastic caps. Minicolpostats are 1.6 cm and have a flat inner surface and have no shielding. Use 15, 20, and 25 mg Ra for small, medium, and large colpostats; use 10 for the minis. Tandems are available in three curvatures. Flange on the tandem avoids slippage past the cervical os, and a keel helps keep it from rotating. A yoke attaches the tandem and colpostats to maintain proper position. Loading of the tandem is 20 - 10 - 10 mgRaEq with Cs-137.
Plastic Fletcher applicators are available to be compatible with CT simulation or MRI.
The Madison system (University of Wisconsin)
- PMID 1526873, 1992 — "High dose rate intracavitary brachytherapy for carcinoma of the cervix: the Madison system: I. Clinical and radiobiological considerations." Stitt JA et al. Int J Radiat Oncol Biol Phys. 1992;24(2):335-48.
- PMID 1526874, 1992 — "High dose rate intracavitary brachytherapy for carcinoma of the cervix: the Madison system: II. Procedural and physical considerations." Thomadsen BR et al. Int J Radiat Oncol Biol Phys. 1992;24(2):349-57.
American Brachytherapy Society (ABS)
Recommend prescribing to Point H - Draw a line connecting the mid-dwell positions of the ovoids and find the point this line intersects the tandem. Follow 2 cm superior (along the tandem) plus the radius of the ovoids, then 2 cm perpendicular to the tandem. Note: This is basically 2 cm above the top of the ovoids.
- ABS General Principles for locally advanced carcinoma of the cervix. (2012) PMID: 22265436 — "American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: general principles." Viswanathan et al. Brachytherapy. 2012 Jan-Feb; 11(1):33-46.
- ABS HDR guidelines. (2012) PMID: 22265437 — "American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: high-dose-rate brachytherapy." Viswanathan et al. Brachytherapy. 2012 Jan-Feb; 11(1):47-52.
- ABS LDR and Pulsed-dose rate guidelines. (2012) - PMID: 22265438 — "American Brachytherapy Society Consensus Guidelines for locally advanced carcinoma of the cervix. Part III: low-dose-rate and pulsed-dose-rate brachytherapy." Lee et al. Brachytherapy. 2012 Jan-Feb; 11(1)53-7.
European Society for Therapeutic Radiation Oncology (ESTRO)
- ESTRO
- 2006 PMID 16403584 -- "Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology." (Potter R, Radiother Oncol. 2006 Jan;78(1):67-77. Epub 2006 Jan 5.)
- Recommendations for 3D dose-volume parameters
- 2005 PMID 15763303 -- "Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV." (Haie-Meder C, Radiother Oncol. 2005 Mar;74(3):235-45.)
- Specification of image-guided GTV and CTV
- 2006 PMID 16403584 -- "Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology." (Potter R, Radiother Oncol. 2006 Jan;78(1):67-77. Epub 2006 Jan 5.)
Good Insertion Characteristics
- AP View
- Tandem midline, unrotated
- Tandem midway between colpostats
- Keel (flange) in close proximity to gold seed markers
- Colpostats high in the fornices along cervix, ideally ~1/3 above flange
- Lateral View
- Tandem bisects the colpostat
- Sufficient anterior and posterior packing
- Foley balloon firmly tugged down
Interstitial brachytherapy
- UC Irvine; 2013 (1996-2009) PMID 22763030 -- "Outcomes of high-dose-rate interstitial brachytherapy in the treatment of locally advanced cervical cancer: long-term results." (Pinn-Bingham M, Int J Radiat Oncol Biol Phys. 2013 Mar 1;85(3):714-20. doi: 10.1016/j.ijrobp.2012.05.033. Epub 2012 Jul 3.)
- Retrospective. 116 patients, cervical cancer (91% Stage IIB-IVA). Combination EBRT 50.4 with 2 interstitial implants HDR 36 Gy. Interstitial hyperthermia in 61%. Concurrent chemotherapy 81%
- Outcome: LRC 85%. 3-year DFS Stage IB 59%, II 67%, Stage III 71%, Stage IVA 57%. 5-year DFS 60%, OS 44%
- Toxicity: acute and late toxicities acceptable
- Conclusion: Locally advanced cervical cancer can achieve excellent outcomes with HDR interstitial brachytherapy
LDR
Dose Prescriptions
- Point A
- Early stage disease (nonbulky Stage I-II): 80-85 Gy
- Advanced stage disease (bulky or Stage IIIB): 85-90 Gy
- Pelvic Sidewall - LDR equivalent of 50-55 Gy (early stage) or 55-60 Gy (advanced stage)
- Early stage disease (nonbulky Stage I-II): 50-55 Gy
- Advanced stage disease (bulky or Stage IIIB): 55-60 Gy
- ABS LDR (2002) - PMID 11777620 — "The American Brachytherapy Society recommendations for low-dose-rate brachytherapy for carcinoma of the cervix." Nag S et al. Int J Radiat Oncol Biol Phys. 2002 Jan 1;52(1):33-48.
- ABS LDR and Pulsed-dose rate guidelines. (2012) - PMID: 22265438 — "American Brachytherapy Society Consensus Guidelines for locally advanced carcinoma of the cervix. Part III: low-dose-rate and pulsed-dose-rate brachytherapy." Lee et al. Brachytherapy. 2012 Jan-Feb; 11(1)53-7.
HDR vs LDR
Equivalent doses
| HDR dose | LDR equivalent |
|---|---|
| 6 Gy x 4 | 32 Gy |
| 6 Gy x 5 | 40 Gy |
- Taiwan (1996) - PMID 8631555 — "Determination of the appropriate fraction number and size of the HDR brachytherapy for cervical cancer." Liu WS et al. Gynecol Oncol. 1996 Feb;60(2):295-300.
- Detroit (1991) - PMID 1938550 — "Comparison of high and low dose rate remote afterloading for cervix cancer and the importance of fractionation." Orton CG et al. Int J Radiat Oncol Biol Phys. 1991 Nov;21(6):1425-34.
- Analysis of 17,000 cervix cancer pts in 56 institutions using HDR.
- Conversion of dose from LDR to HDR, use dose factor of 0.54.
Calculation tools:
- Medical University of Vienna
- link at: http://www.americanbrachytherapy.org/guidelines/index.cfm
- direct link to Excel spreadsheet:
- Spreadsheet #1: (LQ spread sheet) Instructions
- Spreadsheet #2: (Reporting GYN HDR BT sheet) Instructions
Radiobiology
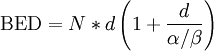
BED for HDR and LDR:
- HDR:
- LDR:
![\mbox{BED} = N*R*t\left [1 + \frac{2R}{\mu*(\alpha/\beta)}*\left (1 - \frac{1-e^{-\mu t}}{\mu*t}\right ) \right ]](../I/m/2bcd13b816571881b8a842f6e3a94fc9.png)
Where N = number of fractions, d = dose per fraction, R = dose rate, t = treatment time (i.e. duration), μ = sublethal damage repair constant, and α/β = characteristic parameter of the cell survival curve from the linear quadratic model.
(from ABS, PMID 10924990)
Problem: What dose/fraction of HDR delivered in six fractions will be equivalent in terms of tumor control to 60 Gy delivered to Point A at 0.55 Gy h−1?
Solution: Assume α/β (tumor) = 10 Gy, μ (tumor) = 0.46 h−1.
Then: BED (LDR) = 60[1 + (2 × 0.55)/(0.46 × 10)] = 74.3
Equating this to the BED for 6 HDR fractions with dose/fraction d gives:
74.3 = 6d(1 + d/10)
Solving this quadratic equation for d gives: d = 7.20 Gy.
Conclusion: 6 fractions of 7.20 Gy with HDR is equivalent in terms of tumor control to 60 Gy delivered at 0.55 Gy h−1.
Other references:
- PMID 10661360 (2000) — "A simple method of obtaining equivalent doses for use in HDR brachytherapy." Nag S et al. Int J Radiat Oncol Biol Phys. 2000 Jan 15;46(2):507-13.
Clinical Comparison
- Meta-analysis; 2010 PMID 20614461 -- "High dose rate versus low dose rate intracavity brachytherapy for locally advanced uterine cervix cancer. (Wang X, Cochrane Database Syst Rev. 2010 Jul 7;(7):CD007563. doi: 10.1002/14651858.CD007563.pub2.)
- Cochrane review. 4 studies, 1265 patients.
- Outcome: no difference in 3-, 5-, and 10-year OS or DSS. No difference for local control, locoregional recurrence, or distant metastases
- Toxicity: No difference for bladder or rectosigmoid toxicity, increased risk for small bowel (RR 3.4, p=0.04)
- Conclusion: Due to potential advantages of HDR, we recommend HDR for all clinical stages of cervix cancer
- India, 1994 (1986-89) - PMID 8276647 — "Low dose rate vs. high dose rate brachytherapy in the treatment of carcinoma of the uterine cervix: a clinical trial." Patel FD et al. Int J Radiat Oncol Biol Phys. 1994 Jan 15;28(2):335-41.
- 482 pts. Randomized two groups (Group I - early stage, brachy only. Group II - EBRT + BT) to HDR vs LDR.
- 5-yr LC 79.7% (LDR) vs 75.8% (HDR). OS: Stage I - 73% vs 78%, Stage II - 62% and 64%, Stage III - 50% and 43. Rectal complications lower for HDR (19.9% vs 6.4%)
HDR
ABS Guidelines
- HDR (2000) - PMID 10924990 — "The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix." Nag S et al. Int J Radiat Oncol Biol Phys. 2000 Aug 1;48(1):201-11.
- General recommendations
- Brachytherapy must be included as a component of radiation therapy for cervical carcinoma
- Good applicator placement must be achieved
- Relative dose of EBRT vs. BT depends on tumor volume, ability to displace bladder and rectum, tumor regression during EBRT, and institutional preference
- Total treatment duration should be <8 weeks
- HDR should be interdigitated with EBRT, such that EBRT is not given on day of BT. If vaginal geometry is optimal, start BT during week #3 and give BT once per week. If tumor volume doesn't allow this, perform 2 BT implants per week after completion of EBRT to stay within 8 week treatment duration limit
- External Beam RT
- HDR fraction size and number depends on EBRT dose (see table below), though individual HDR fraction size should be <7.5 Gy/fx due to concerns about late toxicity
- There is no consensus about midline blocks. If used, should be 4-5cm wide and should not extend to the top of the pelvic field if used at <40 Gy. Care must be taken not to shield common illiac and presecral nodes.
- Midline block position should be reassessed after each implant
- Chemotherapy
- Chemotherapy should be administered concurrently with EBRT, but not with BT
- Insertion technique
- Multiple insertions should be used to allow progressive volume reduction and thus more effective disease coverage
- Optimum applicator placement is critical, and should be done with ultrasound and fluoroscopic guidance
- Appropriate applicator must be chosen for disease geometry: standard ovoids, ring, or Henschke applicator
- If an applicator cannot be accomodated, interstitial implant should be used
- Conscious sedation should be used whenever possible; patient discomfort can lead to suboptimal packing
- Cervical markers should be placed for identification of cervical position and to determine relationship of vaginal applicators to the cervix
- Bladder and rectum should be displaced away from the applicators
- External fixation devices (e.g. perineal bar or clamp/base plate) should be used to prevent movement
- Good quality radiographs should be obtained for treatment planning and dosimetry with each insertion
- Every effort should be made to minimize patient and applicator movement
- Dose specification
- Ideally, dose should be prescribed to individual patient's treatment volume, but there is insufficient information in the literature to establish a better delineated target than Point A
- ABS recommends prescribing to Point H defined as point of intersection of mid-dwell positions of the ovoids with the tandem. Then move superiorly radius of the ovoids (to top of ovoids) + 2 cm, and then 2 cm perpendicularly
- Dose optimization
- Achieving good dose distribution requires both good dose insertion and dose optimization
- Tandem optimization: start 1 cm inferiorly to the superior-most dwell position. Finish 1 cm superior to the surface of the vaginal appliance. Optimization points should fall no further than 1 cm apart along the tandem, and in both lateral directions
- Vaginal optimization should fall at the vaginal surface or specified depth (usually 0.5 cm), and should fall in both lateral directions as not to interfere with tandem optimization
- Dose calculations to organs at risk
- ICRU 38 does not consistently specify location of maximu dose to the organs
- True dose delivered should be calculated using soft tissue (CT or MRI) planning if available
- Nominal rectal and bladder points can be used as per ICRU definitions, and should receive <80% of dose to Point H. Absolute dose should be LDR-equivalent <75 Gy for rectum and <80 Gy for bladder
- Regional lymph nodes: BT component is small compared to EBRT dose, but should be calculated. ICRU 38 Pelvic Wall Point specification should be used. Manchester Point B should not be used
- Dose recommendations
- See table below as a guide
- Point A: LDR equivalent of 80-85 Gy (early stage disease, nonbulky Stage I-II) or 85-90 Gy (advanced stage, Stage IIIB or > 4 cm).
- Pelvic Sidewall: LDR equivalent of 50-55 Gy (early stage) or 55-60 Gy (advanced stage)
- Physical dose delivered will be less for HDR than for LDR due to dose-rate effect
- Quality assurance
- AAPM TG 59 recommendations should be followed
- Interstitial brachytherapy
- Recommended for clinical situations when geometry for intracavitary BT is suboptimal (e.g. bulky lesions, narrow vaginal apex, inability to enter the cervical os, extension to the lateral parametria or pelvic sidewall, and lower vaginal extension)
- Please see the manuscript for further recommendations
- General recommendations
Suggested doses in combination with EBRT:
| EBRT dose | # HDR fractions | HDR dose/fx |
|---|---|---|
| 20 | 6 | 7.5 |
| 20 | 7 | 6.5 |
| 20 | 8 | 6.0 |
| 45 | 5 | 6.0 |
| 45 | 6 | 5.4 |
- ABS HDR guidelines. (2012) PMID: 22265437 — "American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: high-dose-rate brachytherapy." Viswanathan et al. Brachytherapy. 2012 Jan-Feb; 11(1):47-52.
- Image-guided brachytherapy working group
- 2004 PMID 15519788 — "Proposed guidelines for image-based intracavitary brachytherapy for cervical carcinoma: Report from Image-Guided Brachytherapy Working Group." Nag et al. Int J Radiat Oncol Biol Phys. 2004 Nov 15;60(4):1160-72.
HDR Implant Steps
- Perform preliminary bimanual examination for geometry while patient undergoing EBRT
- Induce anesthesia (consider general, conscious sedation, or spinal)
- Consider antibiotic coverage (e.g. Ancef 1 gram)
- Place in lithotomy position
- Examination under anesthesia to assess geometry for implant
- If not, abort and consider interstitial implant
- Prep with betadine and drape (consider "urine cather" to catch stray instruments)
- Place Foley with 7 cc diluted contrast (2 ml contrast + 5 ml saline)
- Fill bladder with saline, using 4-5 big syringes (200-300 ml)
- Open vagina with right angle retractors; weighted speculum may tear friable vaginal mucosa after concurrent chemo-RT
- Use tenaculum to grasp anterior lip of cervix, and maintain tension
- Place 2-3 gold seeds ~5mm into cervix (on x-ray, they will be ~1cm superior to the inferior-most aspect of the cervix)
- Use sound to estimate cervix depth, under ultrasound guidance to avoid perforation
- Once sound is in fundus, grasp exposed portion with a clamp at the cervix, and measure the sound to estimate depth
- Most common location for perforation is posterior endocervix or lower uterine segment
- Dilate cervix
- Leave dilator in place until ready for tandem, to prevent cervical spasm
- Consider Smit sleeve (frequently 60 mm sleeve)
- Insert tandem under ultrasound guidance
- Choose length and angle of tandem based on sound information
- If uterus is retroverted, place tandem to follow the cavity and then gently rotate into anterior position to antervert
- Remove tenaculum
- Insert ovoids or ring
- Lubricating them may help insertion
- Choose largest size that will fit to take advantage of inverse square; however, too large an ovoid may be displaced inferiorly, away from the tumor
- May need ovoids of 2 different sizes if the tumor is asymmetrical
- Typically insert right ovoid, then left ovoid, then lock in place
- If built-in tungsten shields, may provide ~15% dose reduction to the anterior rectal wall
- Verify stable implant placement with ultrasound
- Empty bladder, but keep Foley in place
- Pack anteriorly and posteriorly to ovoids
- Typically 1 inch gauze is used, with DeBakey forceps and/or fingers
- Use lubrication (e.g. premarin cream, surgilube) on the gauze
- Aim for floor and ceiling, but not cephalad to ovoids, so the cervix isn't displaced
- Posterior packing initially to preferentially spare rectum
- Place a stitch in the gauze at the end, to facilitate removal
- Films in O.R. to evaluate implant quality (see above)
- If admitting, consider:
- Activity: bed rest
- Nursing:
- Foley to gravity
- Compression devices to bilateral lower extremities
- Incentive spirometry to bedside; use 10x/hr while awake
- Head of bed at or below 30 degrees
- Diet: clear, advance to low residue as tolerated
- IVF: NS @ 75 ml/hr
- Meds:
- Lovenox 40 mq QD or heparin 5000 units SC Q8
- Pain management (PCA pump or coverage for breakthrough pain)
- Lomotil 1 tab Q6
- Restoril 15 mg Qhs
- Pepcid 20 mg PO BID
- Patient's routine medications
- Send to radiation oncology when stable
- Dictate OP note (e.g. Ms X was taken to the operating room, where she was place under (general, spinal) anesthesia. (ABX) was given. The bladder was filled with sterile saline solution and the uterus was evaluated by ultrasound. The tandem was inserted under ultrasound guidance. The ovoids were placed under direct visualization. The placement of the implant was verfied with ultrasound. Vaginal vault was secured with gauze packing. (There were no complications). The patient was taken to the recovery room in a stable condition.)
- CT sim
- Insert dummy sources
- Consider rectal tube with 20-30 ml barium contrast
Clinical Evidence
- Osaka (Japan)(1983-1989) -- HDR fractional dose 7.5 Gy/fx vs. 6.0 Gy/fx
- Randomized. 165 patients with cervix adenoCA, Stage IA-IV. Treated with 2 separated dose schedules depending on stage. Arm 1) EBRT + BT using 7.5 Gy/fx (either 37.5/5 or 30/4 or 22.5/3) vs. Arm 2) EBRT + BT using 6.0 Gy/fx (either 36/6 or 30/5 or 18/3).
- 5-years; 1994 PMID 7974179 -- "A prospective randomized study concerning the point A dose in high-dose rate intracavitary therapy for carcinoma of the uterine cervix. The final results." (Chatani M, Strahlenther Onkol. 1994 Nov;170(11):636-42.)
- Outcome: 5-year CSS: Stage I 100% vs. 100%, Stage II 82% vs. 85%, Stage III 62% vs. 52%, Stage IV 22% vs. 31% (all NS). No difference in LRF or DM
- Toxicity: No difference
- Conclusion: No difference between the two treatment schedules; small number of fractions at 7.5 Gy/fx may be advantageous due to short duration
Dose limits
- Points specified in ICRU Report 38
- Please see the ICRU report page on more detail about definitions
- Bladder point - on the surface of a Foley balloon filled with 7 cc of contrast; located at center of balloon on AP film, posterior surface of the balloon on a line through midballoon on lateral film
- Rectum point - 0.5 cm posterior to the posterior vaginal wall at the level of the bisection of the T&O. May also use barium + air contrast in rectum
- Vaginal mucosa - at surface of ovoids
- Pelvic sidewall, and external, common, and para-aortic LN points should be reported according to ICRU defintions
- Medical University of Vienna
- Late side effects; 2011 PMID 20385450 -- "Dose-volume histogram parameters and late side effects in magnetic resonance image-guided adaptive cervical cancer brachytherapy." (Georg P, Int J Radiat Oncol Biol Phys. 2011 Feb 1;79(2):356-62. Epub 2010 Apr 10.)
- Retrospective. 141 patients, EBRT and IGBT, +/- chemotherapy. DVH parameters D2cc, D1cc, D0.1cc for rectum, sigmoid, and bladder, as well ICRU rectum and bladder point doses calculated and converted to EQD2. Median F/U 4.2 years
- Outcome: 5-year toxicity rectum 12%, sigmoid 3%, bladder 23%. Mean D2cc rectum 65 Gy (+/- 12 Gy), sigmoid 62 Gy (+/- 12 Gy), and bladder 95 Gy (+/- 22 Gy).
- Conclusion: D2cc and D1cc have good predictive value for rectal toxicity. Recommend rectum D2cc max 75 Gy, sigmoid no recommendation, bladder D2cc max 100 Gy
- Vaginal toxicity; 2010 PMID 20561694 -- "Dose volume parameter D2cc does not correlate with vaginal side effects in individual patients with cervical cancer treated within a defined treatment protocol with very high brachytherapy doses." (Fidarova EF, Radiother Oncol. 2010 Oct;97(1):76-9. Epub 2010 Jun 17.)
- Vaginal D2cc did not correlate with presence or grade of side effects
- Late side effects; 2011 PMID 20385450 -- "Dose-volume histogram parameters and late side effects in magnetic resonance image-guided adaptive cervical cancer brachytherapy." (Georg P, Int J Radiat Oncol Biol Phys. 2011 Feb 1;79(2):356-62. Epub 2010 Apr 10.)
Acute complications
- PMID 10725629 (1960-1992) - "Perioperative and postoperative complications of intracavitary radiation for FIGO stage I-III carcinoma of the cervix." Jhingran A et al. Int J Radiat Oncol Biol Phys. 2000; 46 (5):1177-83
- Retrospective. 7662 intracavitary procedures in 4043 patients for FIGO I-III cervical CA
- 2.8% uterine perforation rate, 14% have fever >101 C during at least 1 admission, 0.1% fatal thromboembolism rate. Perforation did not affect DSS in stage I, II, but did lead to worse prognosis in stage III.
Late complications
- PMID 7635768, 1995 (1960-89) — "Time course and incidence of late complications in patients treated with radiation therapy for FIGO stage IB carcinoma of the uterine cervix." Eifel PJ et al. Int J Radiat Oncol Biol Phys. 1995 Jul 30;32(5):1289-300.
- Retrospective. 1784 pts, FIGO stage IB. Grade 3 or higher complications occurred in 7.7% at 3 yrs and 9.3% at 10 yrs. After 10 yrs, 0.34% per year, so at 20 yrs, 14.4% risk. Risk of rectal complications was the greatest, more than urinary complications.
- Conclusion: low risk of major complications using brachytherapy.
Miscellaneous
- Patterns of care study (2005, 1996-99) - PMID 16099599 — "Patterns of brachytherapy practice for patients with carcinoma of the cervix (1996-1999): a patterns of care study." Erickson B et al. Int J Radiat Oncol Biol Phys. 2005 Nov 15;63(4):1083-92.
External links
- [PDF] (2005) — LDR Intracavitary Brachytherapy Applicators - John Horton, MDACC
- Really nice presentation. Many pictures of applicators, dosimetry, etc.