Wellens' syndrome
Background
- First described in 1982
- Subset of patients fared poorly with medical management of “impending myocardial infarction” (unstable angina)
- Findings can be transient (persists for hours after pain has resolved and then disappears)
Clinical Features
- Symptoms of Myocardial infarction or ischemia
- Symptoms have often resolved at presentation
- May have previous recent episodes of angina or anginal equivalents
- Initial cardiac enzymes are frequently normal or slightly elevated[3][4]
- Cocaine use may cause pseudo-Wellens due to vasospasm without critical stenosis[5]
Differential Diagnosis
- High voltage
- PE
- RBBB
- Hypokalemia
- CNS Injury
- Persistent Juvenile T-wave pattern
- Digitalis Effect
- "Normal variant" STE with biphasic T-wave[6]
- Common in young, healthy, Black males
- Patterns that are NOT found in Wellen's
- High voltage complexes
- Notching at J-point ("fishhook")
- Concave upward ST segment followed by steep drop in T wave
ST Elevation
- Cardiac
- ST-segment elevation myocardial infarction (STEMI)
- Post-MI (ventricular aneurysm pattern)
- Previous MI with recurrent ischemia in same area
- Wellens' syndrome
- Coronary artery vasospasm (eg, Prinzmetal's angina)
- Coronary artery dissection
- Pericarditis
- Myocarditis
- Aortic dissection in to coronary
- Left ventricular aneurysm
- Left ventricular pseudoaneurysm
- Early repolarization
- Left bundle branch block
- Left ventricular hypertrophy (LVH)
- Myocardial tumor
- Myocardial trauma
- RV pacing (appears as Left bundle branch block)
- Brugada syndrome
- Takotsubo cardiomyopathy
- AVR ST elevation
- Other thoracic
- Metabolic
- Drugs of abuse (eg, cocaine, crack, meth)
- Hyperkalemia (only leads V1 and V2)
- Hypothermia ("Osborn J waves")
- Medications
- Tricyclic (TCA) toxicity
- Digoxin
Evaluation
- History of chest pain
- Normal or slightly-elevated cardiac enzymes
- No precordial Q-waves
- Isoelectric or <1mm ST-segment elevation
- Wellens' pattern present in pain-free state
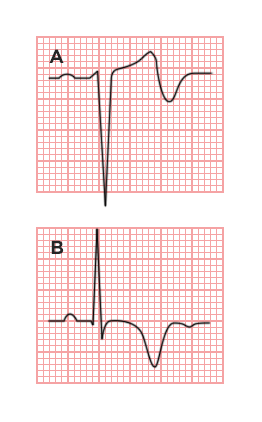
Two T-wave Characteristics (at times terms are reversed in the literature or labeled Type I and II):
- Type A (25%)
- Biphasic T-wave in V2/V3
- Type B (75%)
- Deep, symmetrically inverted T-waves in V2/V3
Note Wellens criteria should not be applied to patients with LVH
Management
- Urgent cardiac catheterization
- Stress testing contraindicated
Disposition
- Admit
See Also
External Links
Video
START_WIDGET996f717d47f2a07f-0END_WIDGET
References
- de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4 Pt 2):730-736.
- Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens' syndrome. American Journal of Emergency Medicine. 2002;20(7):638-643. doi:10.1053/ajem.2002.34800.
- Ünlüer EE et al. Red Flags in Electrocardiogram for Emergency Physicians: Remembering Wellens' Syndrome and Upright T wave in V1. West J Emerg Med. 2012 May; 13(2): 160–162.
- Kannan L and Figueredo VM. Wellens' Syndrome. Jan 1, 2015. N Engl J Med 372;1.
- Dhawan SS. Pseudo-Wellens’ syndrome after crack cocaine use. Can J Cardiol. 2008; 24(5):404.
- Wang, et al. ST-segment elevation in conditions other than acute myocardial infarction. NEJM 2003, 349:2128-2135.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.