Tubo-ovarian abscess
Background
- Typically a complication of PID, although inflammatory bowel, appendicitis, and hematologic nidius have been reported
- Mortality if not ruptured: <1% if treated; 2-4% if untreated
- Infections are often polymicrobial
- Common organisms: Escherichia coli, aerobic streptococci, Bacteroides fragilis, Prevotella, Peptostreptococcus
- N. gonorrhoeae and C. trachomatis are rarely culprit organisms
Clinical Features
- +/-Fever
- Vaginal discharge
- Dyspareunia
- Disproportionate unilateral adnexal tenderness or adnexal mass or fullness
- Suspect in patient who does not respond after 72hr of treatment for PID
Differential Diagnosis
Pelvic Pain
Pelvic origin
- Urinary tract infection
- Ectopic
- Ovarian torsion
- Endometriosis
- Pelvic inflammatory disease
- Cervicitis
- Ectopic pregnancy
- Ovarian torsion
- Spontaneous abortion
- Septic abortion
- Myoma (degenerating)
- Ovarian cyst (rupture)
- Tubo-ovarian abscess
- Mittelschmerz
- Sexual assault/trauma
- Ovarian hyperstimulation syndrome
Abdominal origin
Evaluation
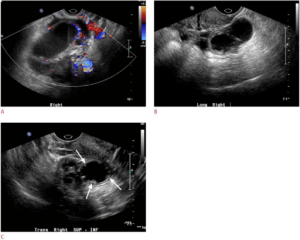
Dilated, complex, fluid-filled tubular structure is consistent with hydro/pyosalpinx (A, B). Short-axis image (C) demonstrates the “cog-wheel” pattern of the endosalpingeal folds, indicative of tubal inflammation in pelvic inflammatory disease with a pyosalpinx or a hydrosalpinx. (arrows).
- CBC
- ESR/CRP
- Transvaginal pelvic ultrasound (Sn 75-82%)
- CT pelvis (Sn 78-100%) - preferred in patients in whom associated GI pathology must be excluded
Management
- OB/GYN consult for possible operative drainage.
- Majority (60-80%) resolve with antibiotics alone
- Predictors of antibiotic treatment failure and possible indications for IR drainage upon admission to Ob[2]
- WBC > 16,000
- TOA size > 5.2 cm
Outpatient
- Ceftriaxone 250mg IM once PLUS doxycycline 100mg PO BID x14 days
- Metronidazole 500mg PO BID x14 days now recommended empirically by European guidelines [3]. Supported by CDC. Definitely give if suspicion of bacterial vaginitis or gynecological instrumentation in preceding 2-3 wks
Inpatient
- Cefoxitin 2gm IV q6hr OR cefotetan 2gm IV q12hr) + doxycycline PO or IV 100mg q12hr OR
- Clindamycin 900mg IV q8h + gentamicin 2mg/kg QD OR
- Ampicillin-sulbactam 3gm IV q6hr + doxycycline 100mg IV/PO q12hr
Disposition
- Decision should be made in conjunction with gynecological colleague
- Patient with fevers, elevated WBC, abscess greater than 5 cm, or systemic toxicity demand admission
- Hemodynamically stable, afebrile patients with a relatively small abscess can be safely discharged with close gynecological follow up on antibiotics
See Also
- PID
References
- https://www.cdc.gov/std/tg2015/pid.htm
- Huma F et al. Inpatient Management of Tubo-Ovarian Abscesses: What Is the Threshold of Parenteral Antibiotic Treatment Failure? Obstetrics & Gynecology: May 2015
- Ross J, Guaschino S, Cusini M, Jensen J, 2017 European guideline for the management of pelvic inflammatory disease. Int J STD AIDS. 2018 Feb;29(2):108-114. doi: 10.1177/0956462417744099. Epub 2017 Dec 4.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.