Truncus arteriosus
Background
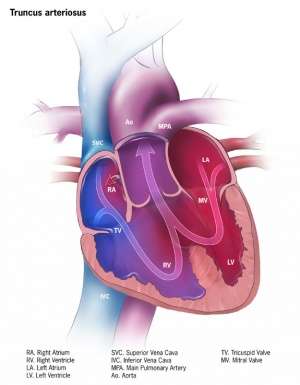
Truncus arteriosus anatomy
- A cyanotic congenital heart defect
- Blood is pumped through a single truncal valve into a truncal artery which gives rise to the aorta and the pulmonary arteries
- Associated with large VSD in most patients
- Incidence ranges from 6 to 10 per 100,000 live births, accounts for 4% of all congenital heart disease [1]
Physiology
- PVR is high in the newborn infant, so there is little left to right shunting at birth
- Over first several weeks of life, PVR drops, left to right shunting increases, leading to heart failure
- Mixing of systemic and pulmonary blood leads to mild to moderate cyanosis
- Pulmonary vascular obstructive disease may develop in surgically uncorrected patients
Clinical Features
- Most present within the first weeks of life with
- Cyanosis
- Pulmonary congestion and heart failure
- Poor feeding, lethargy, signs of respiratory distress (tachypnea, costal-sternal retractions, grunting, and nasal flaring), tachycardia, hyperdynamic precordium, and hepatomegaly
- Cardiovascular findings
- Loud second heart sound
- Prominent ejection click at the apex or left sternal border
- Systolic ejection murmur at the left sternal border
- Bounding peripheral pulses
- Increased pulse pressure
Differential Diagnosis
Congenital Heart Disease Types
- Cyanotic
- Acyanotic
- AV canal defect
- Atrial septal defect (ASD)
- Ventricular septal defect (VSD)
- Cor triatriatum
- Patent ductus arteriosus (PDA)
- Pulmonary/aortic stenosis
- Coarctation of the aorta
- Differentiation by pulmonary vascularity on CXR[2]
- Increased pulmonary vascularity
- Decreased pulmonary vascularity
- Tetralogy of fallot
- Rare heart diseases with pulmonic stenosis
Evaluation
- ECG
- May be normal
- May have evidence of left or right ventricular hypertrophy
- Chest x-ray
- Enlarged cardiac silhouette
- Increased pulmonary vascular markings
- May see absent thymus in patients with TA associated with DiGeorge syndrome
- Echocardiography
Management
- Stabilize cardiopulmonary function prior to surgery
- Diuretic therapy, (eg, furosemide) reduce preload, relieve volume overload and pulmonary congestion
- Inotropic agents (eg, dopamine and dobutamine) improve myocardial contractility
- ACEI reduces afterload
- Noninvasive positive pressure ventilation often used in patients with respiratory distress due to pulmonary congestion
- Supportive care to correct metabolic acidosis, hypoglycemia, and anemia that may contribute to heart failure
- Prostaglandin E1 if patient also has critical coarctation of the aorta
- Primary surgical repair during the neonatal period (less than 30 days of age)
- Improved survival rate at one year of age of >80% vs 15% in uncorrected patients [3]
Disposition
- Admit
See Also
External Links
References
- Reller MD. Prevalence of congenital heart defects in metropolitan Atlanta, 1998-2005. J Pediatr. 2008;153(6):807-13.
- Knipe K et al. Cyanotic congenital heart diseases. Radiopaedia. http://radiopaedia.org/articles/cyanotic-congenital-heart-disease
- Thompson LD. Neonatal repair of truncus arteriosus: continuing improvement in outcomes. Ann Thorac Surg. 2001;72(2):391-5.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.