Transient ischemic attack
Background
- Abbreviation: TIA
- New Definition: a brief episode of neurologic dysfunction caused by focal brain, spinal cord or retinal ischemia, with clinical symptoms typically lasting less than one hour, and without evidence of acute infarction. [1]
- Should be viewed as analogous to unstable angina
- Classic Definition: A sudden, focal neurologic deficit that lasts for less than 24 hours, is presumed to be of vascular origin, and is confined to an area of the brain or eye perfused by a specific artery[1]
- Since 15% of strokes are preceded by TIA, timely eval of high risk conditions like Atrial Fibrillation and Carotid Stenosis is important
Clinical Features
- Focal weakness (Paralysis or paresis of the face, arm, or leg and typically unilateral)
- Dysarthria or dysphasia or aphasia
- Vision changes (Field deficits, blindness, or diplopia)
- Changes in balance or coordination
Differential Diagnosis
Stroke-like Symptoms
- Stroke
- Seizures/postictal paralysis (Todd paralysis)
- Syncope
- Subdural hemorrhage
- Epidural hemorrhage
- Hypoglycemia
- Hyponatremia
- Meningitis/encephalitis
- Hyperosmotic Coma
- Labyrinthitis
- Drug toxicity
- Bell's Palsy
- Complicated migraine
- Meniere Disease
- Demyelinating disease (MS)
- Conversion disorder
- Transient global amnesia
- Giant cell arteritis
- Cerebral sinus thrombosis
Evaluation
Stroke Work-Up
- Labs
- POC glucose
- CBC
- Chemistry
- Coags
- Troponin
- T&S
- ECG
- In large ICH or stroke, may see deep TWI and prolong QT, occ ST changes
- Head CT (non-contrast)
- Also consider:
- CTA brain and neck
- To check for large vessel occlusion for potential thrombectomy
- Determine if there is carotid stenosis that warrants endarterectomy urgently
- Pregnancy test
- CXR (if infection suspected)
- UA (if infection suspected)
- Utox (if ingestion suspected)
- CTA brain and neck
Management
- Little acute management (given normally resolution of symptoms)
- Consider aspirin (once hemorrhage ruled-out)
- Consider dual antiplatelet therapy for high risk TIAs[7]
- Load with ASA 325 mg chewed, followed by ASA 81 mg PO daily
- Load with clopidogrel 300 mg PO followed by 75 mg daily for 3 weeks only
Disposition
ACEP Guidelines[5]
- Level B: In adult patients with suspected TIA, do not rely on current existing risk stratification instruments (eg, age, blood pressure, clinical features, duration of TIA and presence of diabetes [ABCD2] score) to identify TIA patients who can be safely discharged from the ED.
- In contrast to the 2009 AHA/ASA recommendations that were based on limited research, the ABCD2 does not sufficiently identify the short-term risk for stroke to use alone as a risk-stratification instrument.
- Multiple other risk-stratification instruments have been evaluated less frequently than the ABCD2 score. None have demonstrated the ability to identify individual patients at sufficiently low short-term risk for stroke to use alone as a risk-stratification instrument.
- Level B: A rapid ED based diagnostic protocol can be used to safely identify patients at short-term risk for stroke.
- Study based on observation units and outpatient TIA clinics[8]
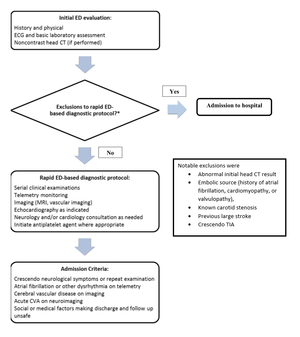
Example of a rapid ED protocol for TIA
Prognosis
ABCD2 Score[9]
- Risk of stroke at 2d, 7d, and 90d from TIA
- Although prognostic, evidence-based admission thresholds have not been determined
- None with score <3 had CVA within one week in study
- Studies have failed to validate the ABCD2 score, and may cause physicians to incorrectly classify ~8% of patients as low risk, with sensitivity of the score for high risk patients only ~30%[10][11]
Scoring
- Age >60yr (1 pt)
- BP (SBP >140 OR diastolic >90) (1 pt)
- Clinical Features
- Isolated speech disturbance (1 pt)
- Unilateral weakness (2 pts)
- Duration of symptoms
- 10-59 min (1 pt)
- >60 min (2 pts)
- Diabetes mellitus (1 pt)
| Points | Stroke Risk | Two Days | Seven Days | 90 Days |
| 0-3 | Low | 1.0% | 1.2% | 3.1% |
| 4-5 | Moderate | 4.1% | 5.9% | 9.8% |
| 6-7 | High | 8.1% | 11.7% | 17.8% |
- According to the 2018 Canadian Heart and Stroke Guideline, the Clinical component of the ABCD2 score is the most important prognostic feature[12]
- Very high risk for recurrent stroke are the following symptoms that have occurred within the last 48 hours
- Transient, fluctuating or persistent unilateral weakness (face, arm and/or leg)
- Transient, fluctuating or persistent language/speech disturbance
- And/or fluctuating or persistent symptoms without motor weakness or language/speech disturbance
- Very high risk for recurrent stroke are the following symptoms that have occurred within the last 48 hours
External Links
See Also
References
- Albers GW, et al. The TIA Working Group. Transient ischemic attack: proposal for a new definition. N Engl J Med. 2002; 347:1713–1716.
- Mullins ME, Schaefer PW, Sorensen AG, Halpern EF, Ay H, He J, Koroshetz WJ, Gonzalez RG. CT and conventional and diffusion-weighted MR imaging in acute stroke: study in 691 patients at presentation to the emergency department. Radiology. 2002 Aug;224(2):353-60.
- Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006; 354(4):387–396.
- Douglas VC, Johnston CM, Elkins J, et al. Head computed tomography findings predict short-term stroke risk after transient ischemic attack. Stroke. 2003;34:2894-2899.
- ACEP Clinical Policy: Suspected Transient Ischemic Attackfull text
- Nederkoorn PJ, Mali WP, Eikelboom BC, et al. Preoperative diagnosis of carotid artery stenosis. Accuracy of noninvasive testing. Stroke. 2002;33:2003-2008.
- Johnston SC, Easton JD, Farrant M, Barsan W, Conwit RA, Elm JJ, Kim AS, Lindblad AS, Palesch YY. Clopidogrel and Aspirin in Acute Ischemic Stroke and High-Risk TIA. N Engl J Med. 2018 Jul 19;379(3):215-225.
- Ross MA, Compton S, Medado P, et al. An emergency department diagnostic protocol for patients with transient ischemic attack: a randomized controlled trial. Ann Emerg Med. 2007;50:109-119
- Johnston SC, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack.Lancet. 2007; 369(9558):283-92.
- Stead LG, Suravaram S. An assessment of the incremental value of the ABCD2 score in the emergency department evaluation of transient ischemic attack. Ann Emerg Med. 2011 Jan;57(1):46-51.
- Ghia D, Thomas P. Low positive predictive value of the ABCD2 score in emergency department transient ischaemic attack diagnoses: the South Western Sydney transient ischaemic attack study. Intern Med J. 2012 Aug;42(8):913-8.
- Boulanger JM, Lindsay MP, Gubitz G, et al. Canadian Stroke Best Practice Recommendations for Acute Stroke Management: Prehospital, Emergency Department, and Acute Inpatient Stroke Care, 6th Edition, Update 2018. Int J Stroke. 2018;:1747493018786616.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.