Acute transfusion reaction
Background
- If concern for fluid overload, may need to transfuse as split pRBCs to tranfuse as slow as 1mL/kg/hr
- Sepsis is most commonly due to yersinia, which is able to grow easily in refrigerated blood
Transfusion Risk Ratios[1]
| Rate | Complication |
| 1:10 | Febrile non-hemolytic transfusion reaction per pool of 5 donor units of platelets (1 pack) |
| 1:100 | Minor allergic reactions (urticaria) |
| 1:300 | Febrile non-hemolytic transfusion reaction per unit of RBC (1 pack) |
| 1:700 | Transfusion-associated circulatory overload per transfusion episode |
| 1:5,000 | Transfusion-related acute lung injury (TRALI) |
| 1:7,000 | Delayed hemolytic transfusion reaction |
| 1:10,000 | Symptomatic bacterial sepsis per pool of 5 donor units of platelets |
| 1:40,000 | Death from bacterial sepsis per pool of 5 donor units of platelets |
| 1:40,000 | ABO-incompatible transfusion per RBC transfusion episode |
| 1:40,000 | Serious allergic reaction per unit of component |
| 1:82,000 | Transmission of hepatitis B virus per unit of component |
| 1:100,000 | Symptomatic bacterial sepsis per unit of RBC |
| 1:500,000 | Death from bacterial sepsis per unit of RBC |
| 1:1,000,000 | Transmission of West Nile Virus |
| 1:3,000,000 | Transmission of HTLV per unit of component |
| 1:3,100,000 | Transmission of hepatitis C virus per unit of component |
| 1:4,700,000 | Transmission of HIV per unit of component |
Clinical Features
- Etiology specific, see ddx below
Differential Diagnosis
Acute allergic reaction
- Allergic reaction/urticaria
- Anaphylaxis
- Angioedema
- Anxiety attack
- Asthma exacerbation
- Carcinoid syndrome
- Cold urticaria
- Contrast induced allergic reaction
- Scombroid
- Shock
- Transfusion reaction
Evaluation
- Workup of hemolytic reaction
- CBC with microscopy differential
- Formal urinalysis with bilirubin
- Haptoglobin, LDH, free hemoglobin
- Serum total and direct bilirubin
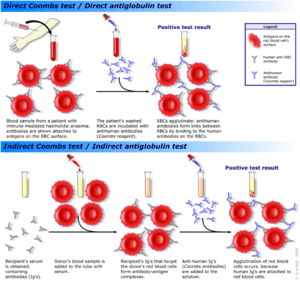
- Coombs test of pre-transfusion and post-transfusion blood
- Consider CXR to help differentiate anaphylaxis, TRALI, TACO
Management
- For all reactions:
- Stop the transfusion (at least temporarily)
- Call the blood bank
- Draw a new type + screen
Disposition
See Also
References
- Wagner, L. Why Should Clinicians Be Concerned about Blood Conservation? ITACCS. 2005 PDF
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.