Torsades de pointes
Background
- Form of polymorphic VTach
- Gradual change in the amplitude of QRS complexes and twisting around isoelectric line
- Associated with congenital or acquired prolonged QT
Common Causes
POINTES mnemonic:
- Phenothiazines
- Other medications (ie TCAs)
- Intracranial bleed
- No known cause (idiopathic)
- Type I antiarrhythmics (quinidine, procainamide, disopyramide)
- Electrolyte abnormalities (hypoK & hypoMg)
- Syndrome of Prolonged QT (aka Long QT Syndrome)
- Other causes:
Clinical Features
- Syncope
- Dizziness, lightheadedness
- Palpitations
- Sudden cardiac arrest
Differential Diagnosis
- Drug induced
- Congenital long QT
- Hypocalcemia
- Hypomagnesemia
- Hypokalemia
- Hypothermia
- POINTES as above
Wide-complex tachycardia
Assume any wide-complex tachycardia is ventricular tachycardia until proven otherwise (it is safer to incorrectly assume a ventricular dysrhythmia than supraventricular tachycardia with abberancy)
- Regular
- Monomorphic ventricular tachycardia
- PSVT with aberrant conduction:
- PSVT with bundle branch block^
- PSVT with accessory pathway
- Atrial flutter with bundle branch block^
- Sinus tachycardia with bundle branch block^
- Accelerated idioventricular rhythm (consider if less than or ~120 bpm)
- Metabolic
- Irregular
- Atrial fibrillation/atrial flutter with variable AV conduction AND bundle branch block^
- Atrial fibrillation/atrial flutter with variable AV conduction AND accessory pathway (e.g. WPW)
- Atrial fibrillation + hyperkalemia
- Polymorphic ventricular tachycardia
^Fixed or rate-related
Evaluation
Workup
- ECG
- BMP, Mg, Phos
Diagnosis
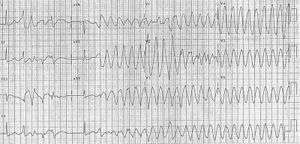
Classic torsades in 12-lead
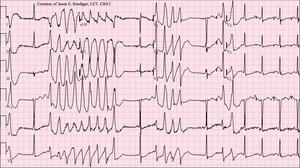
Torsades de Pointes (TdP) in patient with a potassium of 2.4 mmol/L and a magnesium of 1.6mg/dL.
- ECG showing the QRS complexes “twisting” around the isoelectric line
Management
Increasing HR decreases QT interval
- Magnesium sulfate - decreases calcium influx
- 1-2gm IV over 1-2 min, repeat in 5-15min; then 1-2gm/hr (3-10mg/min) drip
- Danger of hypermagnesemia → depressed neuromuscular function and respiratory drive, so monitor closely
- Supplement with K+
- 1-2gm IV over 1-2 min, repeat in 5-15min; then 1-2gm/hr (3-10mg/min) drip
- Isoproterenol - Increases HR / AV conduction
- 2-8 mcg/min
- Target HR > 90 bpm
- Overdrive Pacing - Atrial > Ventricular pacing
- Goal HR 90-120
- Note: Not a treatment for TdP, but useful in maintaining sinus rhythm
- Defibrillation / synchronized cardioversion - Patient in extremis
- AVOID amiodarone and procainamide, which may worsen prolonged QT
- Lidocaine (a class Ib antiarrhythmic drug) shortens the QT interval and may be effective especially for drug-induced torsades de pointes.
Disposition
- Admit
See Also
References
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.