Thoracotomy
Indications
ED Thoracotomy
Penetrating chest trauma
- Signs of Life (pre or in-hospital)
- Pulse, BP, pupil reactivity, purposeful movement, respiratory effort
- Cardiac Activity
- PEA is acceptable
- Unresponsive hypotension
- SBP<70 despite treatment
Blunt chest trauma
- Witnessed signs of life (pre or in-hospital)
- Rapid exsanguination
- >1000-1500mL initial drainage or >200mL/hr from Chest tube
- Consider for exsanguinating abdominal vascular injuries with witnessed signs of life
- Unresponsive hypotension
- SBP<70 despite treatment
OR Thoracotomy
- Thoracoabdominal trauma patients with persistent SBP < 70-80 despite aggressive resuscitation
- Evidence of cardiac tamponade or progressively increasing hemothorax
- Chest tube drainage
- > 20ml/kg initially (> 1500ml in adult)
- > 3 ml/kg/hr for 2-4hrs (> 200 mL/hr for 2-4hr in adult)
- Persistent bleeding > 7 ml/kg/hr
- Persistent air leak (bronchopleural fistula)
Goals
- Release tamponade
- Control intrathoracic/cardiac bleeding
- Control air embolism
- Cardiac massage
- Temporary occlusion of descending aorta (optimize flow to brain and heart)
Contraindications
- No absolute contraindications to ED thoracotomy (emergent procedure)
- Relative Contraindications
- Blunt injury without witness cardiac activity
- Penetrating abdominal trauma without cardiac activity
- Non-traumatic cardiac arrest
- Severe head injury
- Severe multi-system injury
- Improper Setting
- Understaffed ER/Improperly trained staff/Insufficient equipment
Equipment Needed
- PPE
- Thoracotomy Tray
- Rib Spreader
- #10 or #21 Scalpel, Scissors, Forceps
- Vascular Clamps, Curved Artery Forceps, Needle Driver
- Internal Defibrillation Paddles
- Skin Stapler, Suture Material
Procedure
ED thoracotomy
- Intubate and place NGT
- Always start with left-sided approach (even if penetrating injury is on right side)
- If possible, should have concurrent right sided chest tube being placed
- Incise from sternum to to posterior axillary line (4th or 5th intercostal space)
- Cut through skin, soft tissue, and muscle in one pass
- May scissors can be used to cut the intercostal muscle
- Rib spreader with rachet bar down
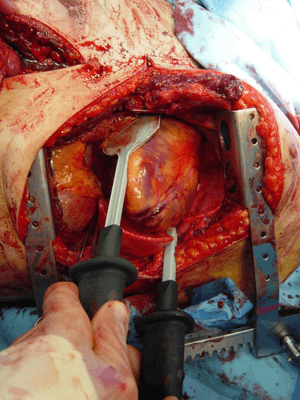
- Push lung out of way to access pericardium
- Pericardiotomy
- Pick up pericardium just anterior to phrenic nerve
- Incise from apex to root of aorta parallel to phrenic nerve
- Inspect myocardium for lacerations
- Digital occlusion
- Skin stapler - if coronary artery stapled, it can be removed in the OR
- Foley catheter with purse-string suture around it (closes wound when foley removed)
- Horizontal mattress (can be difficult with beating heart)
- Cardiac Massage
- one-handed vs two-handed
- Intracardiac epinephrine
- Internal Defibrillation
- Lower voltages than external defibrillation
- Start at 5J to a max of 50J
- Cross Clamp Aorta
- Up to 30 min is tolerated
- Indicated after persistent hypotension after pericardiotomy and fluid resus
- Aorta posterior to NGT
- Autotransfuse thoracic blood
- If no evidence of injury to L-side, but possible R-sided injury, extend to R side (clam shelling)
Complications
Comments
- Survival rates are uniformly poor with guidelines reporting:[1]
- Blunt trauma survival as great as 2%
- Penetrating trauma survival as great 16%
- Meta-analysis reports overall rates closer to 1.5% with favorable neurologic outcome[2]
- Best outcomes occur if the patient arrested less than 15 minutes before the procedure.
- For blunt trauma survival rate may be closer to 0.8%[2]
See Also
External Links
References
- Hopson LR et al. Guidelines for withholding or termina- tion of resuscitation in prehospital traumatic cardiopulmonary arrest: Joint Position Statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. J Am Coll Surg. 2003; 196:106.
- Slessor D, Hunter S. To be blunt: are we wasting our time? Emergency department thoracotomy following blunt trauma: a systematic review and meta-analysis. Ann Emerg Med. 2015 Mar;65(3):297-307
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.