Sympathetic crashing acute pulmonary edema (SCAPE)
Background
- Different from acute CHF exacerbation or hypotensive cardiogenic shock, which do not have sympathetic overdrive
- Patients can decompensate rapidly, so rapid intervention required
- Patients are generally more fluid depleted despite "wet" lungs, so do not give diuretics
- Usually history of poorly controlled hypertension
- Acute afterload increase causes pulmonary edema and poor peripheral perfusion
- Sympathetic surge occurs as a result of decreased systemic perfusion
- Afterload further increases and patient rapidly decompensates
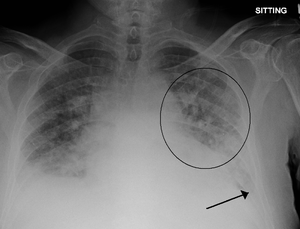
Pulmonary edema with small pleural effusions on both sides.
Clinical Features
- Rales, crackles
- SBP >180 mmHg
- Tachycardia
Differential Diagnosis
Pulmonary Edema Types
Noncardiogenic pulmonary edema
- Negative pressure pulmonary edema
- Upper airway obstruction
- Reexpansion pulmonary edema
- Strangulation
- Neurogenic causes
- Iatrogenic fluid overload
- Multiple blood transfusions
- IV fluid
- Inhalation injury
- Pulmonary contusion
- Aspiration pneumonia and pneumonitis
- Other
- High altitude pulmonary edema
- Hypertensive emergency
- ARDS
- Sympathetic crashing acute pulmonary edema (SCAPE)
- Immersion pulmonary edema
- Hantavirus pulmonary syndrome
- Missed dialysis in kidney failure
Evaluation
- CBC (rule out anemia)
- Chem
- ECG
- CXR - signs of pulmonary congestion may not show for hours after acute flash pulmonary edema, so normal CXR is frequently seen
- Cephalization
- Interstitial edema
- Pulmonary venous congestion
- Pleural effusion
- Alveolar edema
- Cardiomegaly
- Troponin
- Echocardiography
- Bedside to assess global function, B lines, assessment of IVC
- Formal TTE/TEE
- Consider arterial line monitoring for titration of NTG
Brain natriuretic peptide (BNP)[1]
- Measurement
- <100 pg/mL: Negative for acute CHF (Sn 90%, NPV 89%)
- 100-500 pg/mL: Indeterminate (Consider differential diagnosis and pre-test probability)
- >500 pg/mL: Positive for acute CHF (Sp 87%, PPV 90%)
- Combination of BNP with clinician judgment 94% sensitive 70% specific (compared to 49% sn and 96% spec clinical judgement alone) [2]
Management
Vasodilate arterial side, while maintaining oxygenation
- BiPAP with PEEP of 8 mmHg
- Titrate PEEP quickly to 12
- High dose nitroglycerin over 2 min (at these doses, nitroglycerin has vasodilation > venodilation[6])
- Goal BP at the patient's norm
- Load 800 mcg over 2 min (may start at 100 mcg/min, then titrate rapidly to 400 mcg/min for 2 min)
- Then start maintenance at 100 mcg/min, titrate up as needed
- NOTE: it takes time to set up nitroglycerin drip, so consider SL nitroglycerin in interim
- 0.4mg tab during 5 min = ~80 mcg/min (2 tabs = ~160 mcg/min, etc.)
- Difficult to titrate if giving more than 1-2 tabs
- Patients are likely more dehydrated that overloaded but should be recurrently volume assessed
- Consider captopril 12.5 - 25mg SL for continuation of afterload reduction[7]
- Wean CPAP after sustained BP at patient's baseline
- Decrease FiO2 to 40%
- Wean PEEP down 2 cm H2O q10 min
- At 5 cmH2O, trial of NC
Other Interventions
- Furosemide
- Targets kidneys which are poorly perfused in BOTH hypotension and catecholamine surge
- Consider waiting until BiPAP and nitroglycerin control hypertension first
- Nitroprusside, alternative when insufficient response to NTG
- Start 0.5 mcg/kg/min, titrate to blood pressure
- Max 10 mcg/kg/min for x10 min
- Cyanide toxicity risk increases proportionately with infusion rate as well as length of time[8]
- If intubation required, consider delayed sequence intubation
Disposition
- Admit
See Also
External Links
References
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-167. doi:10.1056/NEJMoa020233.
- McCullough et al. B-Type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from breathing not properly (BNP) multinational study. Circulation. 2002:DOI: 10.1161/01.CIR.0000025242.79963.4
- Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J. 2006 Feb. 27(3):330-7.
- Kragelund C, Gronning B, Kober L, Hildebrandt P, Steffensen R. N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med. 2005 Feb 17. 352(7):666-75.
- Moe GW, Howlett J, Januzzi JL, Zowall H,. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007 Jun 19. 115(24):3103-10.
- Haber et al. Bolus intravenous nitroglycerin predominantly reduces afterload in patients with excessive arterial elastance. J Am Coll Cardiol. 1993;22(1):251-257.
- Hamilton RJ, Carter WA, Gallagher JE. Rapid Improvement of acute pulmonary edema with sublingual captopril. Acad Emerg Med 1996; 3: 205-12.
- GlobalRPH. Nitroprusside (Nipride®). http://www.globalrph.com/nitroprusside_dilution.htm
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.