Superior vena cava syndrome
Background
- External compression by extrinsic malignant mass causes majority of cases
- Thrombus in SVC from indwelling catheter/pacemaker is increasingly more common as cause
- Other causes include benign tumors, aortic aneurysm, infections, and fibrosing mediastinitis[1]
- Rarely constitutes an emergency
- Gradual process; collaterals dilate to compensate for the impaired flow
- Exception is neurologic abnormalities due to increased ICP, laryngeal edema causing stridor, decreased cardiac output
Clinical Features
- Facial swelling
- Worse in morning, gets better as day progresses
- Headache
- Cyanosis
- Dyspnea
- Cough
- Arm swelling
- Distended neck/chest wall veins
- Telangiectasia
- Neurologic abnormalities (rare)
Differential Diagnosis
Facial Swelling
Related to Local Tumor Effects
- Malignant airway obstruction
- Bone metastases and pathologic fractures
- Malignant spinal cord compression
- Malignant Pericardial Effusion and Tamponade
- Superior vena cava syndrome
Related to Biochemical Derangement
- Hypercalcemia of malignancy
- Hyponatremia due to SIADH
- Adrenal insufficiency
- Tumor lysis syndrome
- Carcinoid syndrome
Related to Hematologic Derangement
Related to Therapy
- Chemotherapy-induced nausea and vomiting
- Cytokine release syndrome
- Chemotherapeutic drug extravasation
- Differentiation syndrome (retinoic acid syndrome) in APML
- Stem cell transplant complications
- Catheter-related complications
- Tunnel infection
- Exit site infection
- CVC obstruction (intraluminal or catheter tip thrombosis)
- Catheter-related venous thrombosis
- Fracture of catheter lumen
- Oncologic therapy related adverse events
Evaluation
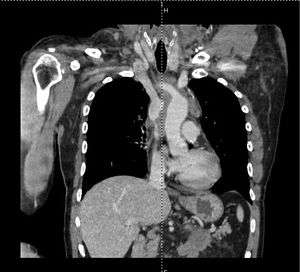
CT chest showing right lung tumor compressing SVC
- CT with IV contrast
- Recommended imaging modality (assesses patency of the SVC, evaluate etiology mass vs. thrombus)
- CXR
- Shows mediastinal mass or parenchymal lung mass (10% of patients)
Management
- Elevate head of bed
- Assess for and treat elevated intracranial pressure
- Use IVs placed in lower extremities to avoid further SVC venous congestion[2]
- Corticosteroids and loop diuretics have questionable efficacy and should be held until ordered by admitting team[3]
- Intravascular stent, consult IR
- If malignancy
- Mediastinal radiation, consult oncology/radiation oncology
- If thrombus
- Anticoagulation, catheter removal, consider thrombolytics
Disposition
- Admit to ICU, with plan for airway monitoring and tissue biopsy
References
- Nickloes TA, Lopez Rowe V, Kallab AM, Dunlap AB (28 March 2018). "Superior Vena Cava Syndrome". Medscape
- Chaudhary K, Gupta A, Wadhawan S, Jain D, Bhadoria P. Anesthetic management of superior vena cava syndrome due to anterior mediastinal mass. J Anaesthesiol Clin Pharmacol [serial online] 2012 [cited 2016 Jul 19];28:242-6. Available from: http://www.joacp.org/text.asp?2012/28/2/242/94910.
- McCurdy M et al. Oncologic emergencies, part I: spinal cord compression, superior vena cava syndrome, and pericardial effusion. Emergency Medicine Practice. 2010; 12(2):7-10.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.