Stroke (main)
Background
- Vascular injury that reduces cerebral blood flow to specific region of brain causing neuro impairment
- Accurate determination of last known time when patient was at baseline is essential
- In-hospital mortality of 5-10% for ischemic stroke and 40-60% for hemorrhagic stroke
- Only 10% of stroke survivors will recover completely
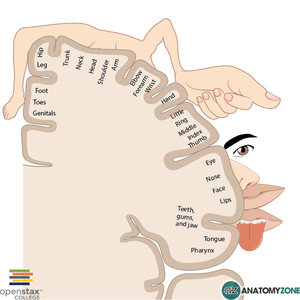
Sensory Homonculus - courtesy AnatomyZone.com
Ischemic stroke causes (87% of all strokes)
- Thrombotic (80% of ischemic CVA)
- Atherosclerosis
- Vasculitis
- Vertebral and carotid artery dissection
- Often preceded by yoga, spinal manipulation, coughing, vomiting
- Polycythemia
- Hypercoagulable state (oral contraceptives, antiphospholipid antibodies, protein S and C deficiencies, sickle cell anemia)
- Infection
- Toxicologic exposure (cocaine, amphetamines, etc.)
- Embolic (20% of ischemic CVA)
- Valvular vegetations
- Mural thrombi
- Arterial-arterial emboli from proximal source (ex. amaurosis fugax -> emboli from a proximal carotid artery plaque embolizes to the ophthalmic artery, causing transient monocular blindness)
- Fat emboli
- Septic emboli
- Hypoperfusion
- Cardiac failure resulting in systemic hypotension
Hemorrhagic stroke causes (13% of all strokes)
- Intracerebral
- Hypertension
- Cerebral amyloid angiopathy (usually found in elderly, tends to be lobar in nature)[1]
- Anticoagulation
- Vascular malformations (e.g. AVM, moyamoya
- Cocaine use
- Subarachnoid hemorrhage
- Berry aneurysm rupture
- Arteriovenous malformation
Clinical Features
Internal Carotid Artery
- Tonic gaze deviation towards lesion
- Global aphasia, dysgraphia, dyslexia, dyscalculia, disorientation (dominant lesion)
- Spatial or visual neglect (non-dominant lesion)
Anterior Cerebral Artery (ACA)
Signs and Symptoms:
- Contralateral sensory and motor symptoms in the lower extremity (sparing hands/face)
- Urinary and bowel incontinence
- Left sided lesion: akinetic mutism, transcortical motor aphasia
- Right sided lesion: Confusion, motor hemineglect
- Presence of primitive grasp and suck reflexes
- May manifest gait apraxia
Middle Cerebral Artery (MCA)

Patient with stroke (forehead sparing).
Signs and Symptoms:
- Hemiparesis, facial plegia, sensory loss contralateral to affected cortex
- Motor deficits found more commonly in face and upper extremity than lower extremity
- Dominant hemisphere involved: aphasia
- Wernicke's aphasia (receptive aphasia) -> patient unable to process sensory input and don't understand verbal communication
- Broca's aphasia (expressive aphasia) -> patient unable to communicate verbally, even though understanding may be intact
- Nondominant hemisphere involved: dysarthria (motor deficit of the mouth and speech muscles; understanding intact) w/o aphasia, inattention and neglect side opposite to infarct
- Contralateral homonymous hemianopsia
- Gaze preference toward side of infarct
- Agnosia (inability to recognize previously known subjects)
Posterior circulation
- Blood supply via the vertebral artery
- Branches include, AICA, Basilar artery, PCA and PICA
Signs and Symptoms:
- Crossed neuro deficits (i.e., ipsilateral CN deficits w/ contralateral motor weakness)
- Multiple, simultaneous complaints are the rule (including loss of consciousness, nausea/vomiting, alexia, visual agnosia)
- 5 Ds: Dizziness (Vertigo), Dysarthria, Dystaxia, Diplopia, Dysphagia
- Isolated events are not attributable to vertebral occlusive disease (e.g. isolated lightheadedness, vertigo, transient ALOC, drop attacks)
- Approximately 25% associated with aortic dissection
Basilar artery
Signs and Symptoms:
- Quadriplegia, coma, locked-in syndrome
- "Crossed signs" in which a patient has unilateral cranial nerve deficits but contralateral hemiparesis and hemisensory loss suggest brainstem infarction
- Sparing of vertical eye movements (CN III exits brainstem just above lesion)
- Thus, may also have miosis b/l
- One and a half syndrome (seen in a variety of brainstem infarctions)
- "Half" - INO (internuclear ophthalmoplegia) in one direction
- "One" - inability for conjugate gaze in other direction
- Convergence and vertical EOM intact
- Medial inferior pontine syndrome (paramedian basilar artery branch)
- Medial midpontine syndrome (paramedian midbasilar artery branch)
- Medial superior pontine syndrome (paramedian upper basilar artery branches)
Superior Cerebellar Artery (SCA)
- ~2% of all cerebral infarctions[2]
- May present with nonspecific symptoms - nausea/vomiting, dizziness, ataxia, nystagmus (more commonly horizontal)[3]
- Lateral superior pontine syndrome
- Ipsilateral ataxia, nausea/vomiting, nystagmus, Horner syndrome, conjugate gaze paresis
- Contralateral loss of pain/temperature in face/extremities/trunk, and loss of proprioception/vibration in LE > UE
Posterior Cerebral Artery (PCA)
Signs and Symptoms:
- Common after CPR, as occipital cortex is a watershed area
- Unilateral headache (most common presenting complaint)
- Visual field defects (contralateral homonymous hemianopsia, unilateral blindness)
- Visual agnosia - can't recognize objects
- Possible macular sparing if MCA unaffected
- Motor function is typically minimally affected
- Lateral midbrain syndrome (penetrating arteries from PCA)
- Medial midbrain syndrome (upper basilar and proximal PCA)
Anterior Inferior Cerebellar Artery (AICA)
- Lateral inferior pontine syndrome
- Ipsilateral facial paralysis, loss of corneal reflex (CN VII)
- Ipsilateral loss of pain/temperature (CN V)
- Nystagmus, nausea/vomiting, vertigo, ipsilateral hearing loss (CN VIII)
- Ipsilateral limb and gait ataxia
- Ipsilateral Horner syndrome
- Contralateral loss of pain/temperature in trunk and extremities (lateral spinothalamic)
Posterior Inferior Cerebellar Artery (PICA)
Signs and Symptoms:
- Lateral medullary/Wallenberg syndrome
- Ipsilateral cerebellar signs, ipsilateral loss of pain/temperature of face, ipsilateral Horner syndrome, ipsilateral dysphagia and hoarseness, dysarthria, vertigo/nystagmus
- Contralateral loss of pain/temp over body
- Also caused by vertebral artery occlusion (most cases)
Internal Capsule and Lacunar Infarcts
- May present with either lacunar c/l pure motor or c/l pure sensory (of face and body)[4]
- Pure c/l motor - posterior limb of internal capsule infarct
- Pure c/l sensory - thalamic infarct (Dejerine and Roussy syndrome)
- C/l motor plus sensory if large enough
- Clinically to cortical large ACA + MCA stroke - the following signs suggest cortical rather than internal capsule[5]:
- Gaze preference
- Visual field defects
- Aphasia (dominant lesion, MCA)
- Spatial neglect (non-dominant lesion)
- Others
- Ipsilateral ataxic hemiparesis, with legs worse than arms - posterior limb of internal capsule infarct
- Dysarthria/Clumsy Hand Syndrome - basilar pons or anterior limb of internal capsule infarct
Anterior Spinal Artery (ASA)
Superior ASA
- Medial medullary syndrome - displays alternating pattern of sidedness of symptoms below
- Contralateral arm/leg weakness and proprioception/vibration
- Tongue deviation towards lesion
Differential Diagnosis
Stroke-like Symptoms
- Stroke
- Seizures/postictal paralysis (Todd paralysis)
- Syncope
- Subdural hemorrhage
- Epidural hemorrhage
- Hypoglycemia
- Hyponatremia
- Meningitis/encephalitis
- Hyperosmotic Coma
- Labyrinthitis
- Drug toxicity
- Bell's Palsy
- Complicated migraine
- Meniere Disease
- Demyelinating disease (MS)
- Conversion disorder
- Transient global amnesia
- Giant cell arteritis
- Cerebral sinus thrombosis
Weakness
- Neuromuscular weakness
- Upper motor neuron:
- Lower motor neuron:
- Spinal and bulbar muscular atrophy (Kennedy's syndrome)
- Spinal cord disease:
- Infection (Epidural abscess)
- Infarction/ischemia
- Trauma (Spinal Cord Syndromes)
- Inflammation (Transverse Myelitis)
- Degenerative (Spinal muscular atrophy)
- Tumor
- Peripheral nerve disease:
- NMJ disease:
- Muscle disease:
- Rhabdomyolysis
- Dermatomyositis
- Polymyositis
- Alcoholic myopathy
- Non-neuromuscular weakness
- Can't miss diagnoses:
- ACS
- Arrhythmia/Syncope
- Severe infection/Sepsis
- Hypoglycemia
- Periodic paralysis (electrolyte disturbance, K, Mg, Ca)
- Respiratory failure
- Emergent Diagnoses:
- Symptomatic Anemia
- Severe dehydration
- Hypothyroidism
- Polypharmacy
- Malignancy
- Other causes of weakness and paralysis
- Acute intermittent porphyria (ascending weakness)
- Can't miss diagnoses:
Evaluation
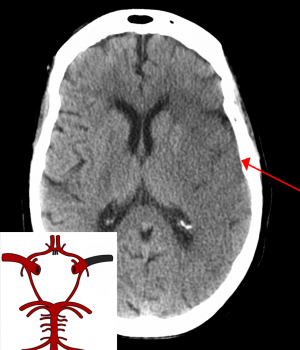
Ischemic stroke with CT showing early signs of a middle cerebral artery stroke with loss of definition of the gyri and grey white boundary.

Hemorrhagic stroke (i.e. spontaneous intracranial hemorrhage).
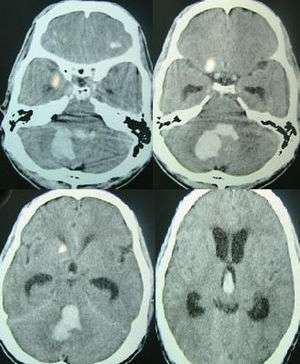
Hemorrhagic stroke in the posterior fossa.
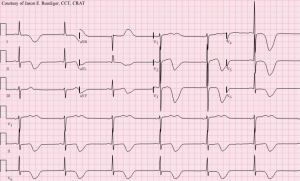
12-lead ECG of a patient with acute stroke, showing large deeply inverted T-waves.
Always obtain blood glucose, which is commonly overlooked (more embarrassing if you give tPA) Find out last known normal of affected deficit and write it down in chart
Stroke Work-Up
- Labs
- POC glucose
- CBC
- Chemistry
- Coags
- Troponin
- T&S
- ECG
- In large ICH or stroke, may see deep TWI and prolong QT, occ ST changes
- Head CT (non-contrast)
- Also consider:
- CTA brain and neck
- To check for large vessel occlusion for potential thrombectomy
- Determine if there is carotid stenosis that warrants endarterectomy urgently
- Pregnancy test
- CXR (if infection suspected)
- UA (if infection suspected)
- Utox (if ingestion suspected)
- CTA brain and neck
MR Imaging (for Rule-Out CVA or TIA)
- MRI Brain with DWI, ADC (without contrast) AND
- Cervical vascular imaging (ACEP Level B in patients with high short-term risk for stroke):[9]
- MRA brain (without contrast) AND
- MRA neck (without contrast)
- May instead use Carotid CTA or US (Carotid US slightly less sensitive than MRA)[10] (ACEP Level C)
Large Vessel Occlusion - Thrombectomy
VAN Score
- NIHSS score ≥ 6 is nearly 100% sensitive for emergent large vessel occlusion, which may be amenable to thrombectomy[13]
- VAN score is just as sensitive, but also may be more specific (~90%)
- Weakness must be present, plus one or all of the VAN to be VAN positive
- Weakness qualifying findings -- if no weakness, the pt is VAN negative
- Mild (minor drift)
- Moderate (severe drift—touches or nearly touches ground)
- Severe (flaccid or no antigravity)
- Visual disturbance qualifying findings
- Field cut (which side) (4 quadrants)
- Double vision (ask patient to look to right then left; evaluate for uneven eyes)
- Blind new onset
- Aphasia qualifying findings
- Expressive (inability to speak or paraphasic errors); do not count slurring of words (repeat and name 2 objects)
- Receptive (not understanding or following commands) (close eyes, make fist)
- Mixed
- Neglect qualifying findings
- Forced gaze or inability to track to one side
- Unable to feel both sides at the same time, or unable to identify own arm
- Ignoring one side
- Weakness qualifying findings -- if no weakness, the pt is VAN negative
- If VAN positive, CT and CTA of the head should be ordered for consideration of thrombectomy plus/minus tPA
- Weakness must be present, plus one or all of the VAN to be VAN positive
Management
- Depends on type
- Ischemic vs Hemorrhagic
- Acute vs subacute vs old
- Due to risk for hemorrhagic transformation, there is no role in acute completed stroke for:
- Dual antiplatelet therapy (as opposed in select cases of TIA)
- Anticoagulation, with or without atrial fibrillation
Disposition
- Admit for acute or subacute stroke
See Also
External Links
References
- Itoh Y, Yamada M, Hayakawa M, Otomo E, Miyatake T. Cerebral amyloid angiopathy: a significant cause of cerebellar as well as lobar cerebral hemorrhage in the elderly. J Neurol Sci. 1993 Jun;116(2):135-41.
- Macdonell RA, Kalnins RM, Donnan GA. Cerebellar infarction: natural history, prognosis, and pathology. Stroke. 18 (5): 849-55.
- Lee H, Kim HA. Nystagmus in SCA territory cerebellar infarction: pattern and a possible mechanism. J Neurol Neurosurg Psychiatry. 2013 Apr;84(4):446-51.
- Rezaee A and Jones J et al. Lacunar stroke syndrome. Radiopaedia. http://radiopaedia.org/articles/lacunar-stroke-syndrome.
- Internal Capsule Stroke. Stanford Medicine Guide. http://stanfordmedicine25.stanford.edu/the25/ics.html
- Mullins ME, Schaefer PW, Sorensen AG, Halpern EF, Ay H, He J, Koroshetz WJ, Gonzalez RG. CT and conventional and diffusion-weighted MR imaging in acute stroke: study in 691 patients at presentation to the emergency department. Radiology. 2002 Aug;224(2):353-60.
- Suarez JI, Tarr RW, Selman WR. Aneurysmal subarachnoid hemorrhage. N Engl J Med. 2006; 354(4):387–396.
- Douglas VC, Johnston CM, Elkins J, et al. Head computed tomography findings predict short-term stroke risk after transient ischemic attack. Stroke. 2003;34:2894-2899.
- ACEP Clinical Policy: Suspected Transient Ischemic Attackfull text
- Nederkoorn PJ, Mali WP, Eikelboom BC, et al. Preoperative diagnosis of carotid artery stenosis. Accuracy of noninvasive testing. Stroke. 2002;33:2003-2008.
- Albers GW, Marks MP, Kemp S, et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N Engl J Med. 2018;378(8):708-718.
- Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000;355(9216):1670-4.
- Teleb MS, Ver Hage A, Carter J, et al Stroke vision, aphasia, neglect (VAN) assessment—a novel emergent large vessel occlusion screening tool: pilot study and comparison with current clinical severity indices Journal of NeuroInterventional Surgery 2017;9:122-126.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.