Nasal septal hematoma
Background
- Submucosal vessels disrupted
- Blood accumulates between perichondrium and cartilaginous septum
- Requires immediate incision and drainage to prevent nasal septum necrosis
- Can lead to saddle nose deformity, nasal septum abscess
- May be complicated by necrosis and perforation
- Suspect septum abscess in patient who presents late after facial trauma with systemic symptoms
- Ensure thorough examination of both nares - Nasal septum cartilage easily fractures (form bilateral hematomas)
Clinical Features
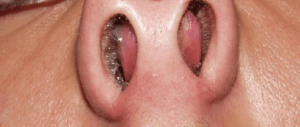
Bilateral nasal septal hematoma
- Adults present with significant facial trauma and nasal fracture
- Dark purple hematoma against septum
- Common symptoms in peds, usually within first 24-72 hrs with even minor nasal trauma, include:
- Nasal obstruction (95%)
- Pain (50%)
- Rhinorrhea (25%)
- Fever (25%)
Differential Diagnosis
Evaluation
- Usually clinical
- Oxymetazoline will not change size of hematoma, as opposed to typical soft tissue edema from trauma
Management
- Place lidocaine-soaked cotton pledgets in nose for 5min
- Achieve visualization with nasal speculum
- Make horizontal incision superficially through the mucosa and the perichondrium
- Ensure that you do not incise the cartilagenous septum
- Evacuate clot with Frazier suction or forceps
- Insert single 1/8in iodoform gauze wick into the incision to avoid premature closure
- Perform bilateral anterior nasal packing with nasal tampons coated with topical antibiotics
- Prevents reaccumulation of clot and keeps septum midline
- Give oral antibiotics (cover S. aureus, H. flu, S. pneumo)
- Amoxicillin-clavulanate for uncomplicated
- Clindamycin if abscess suspected
- Amoxicillin-clavulanate for uncomplicated
Disposition
- Discharge with 24hr ENT or ED follow-up
See Also
External Links
- NEJM procedure video: https://www.youtube.com/watch?v=J5xzYyxgQ0g
References
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.