Sexually transmitted diseases
Background
Bacterial Vaginosis
First Line Therapy[2]
- Metronidazole 500 mg PO BID for 7 days OR
- Metronidazole gel 0.75%, one full applicator (5 g) intravaginally, qd for 5 days OR
- Clindamycin cream 2%, one full applicator (5 g) intravaginally qHS for 7 days
Alternative Regimin
- Tinidazole 2 g PO qd for 2 days OR
- Tinidazole 1 g PO qd for 5 days OR
- Clindamycin 300 mg PO BID for 7 days OR
- Clindamycin ovules 100 mg intravaginally qHS for 3 days (do not use if patient has used latex condom in last 72 hrs)
Pregnant
- Metronidazole 250mg PO q8h x 7 days[3]
- Metronidazole 2g PO x 1 dose is also acceptable[3]
- Multiple studies have not demonstrated teratogenicity from metronidazole use[3]
Cervicitis
Treatment covers both gonorrhea and chlamydia
Uncomplicated Infection
- Ceftriaxone 250mg IM once PLUS
- Azithromycin 1g PO once OR
- Doxycycline 100mg PO BID x 14 days (7 days for gonorrhea, 14 days for chlamydia)[4]
Cephalosporin Allergy
- Azithromycin 2g PO once PLUS
- Gentamicin 240mg IM once[5]
- In theory this high dose macrolide will provide treatment for both GC and Chlamydia
Partner treatment
- Cefixime 400mg PO once PLUS
- Azithromycin 1g PO once OR
- Doxycycline 100mg PO BID x 7 days
Associated Bacterial Vaginosis or Trichomonas vaginalis
Pregnant
Only treat if the patient is symptomatic and avoid breast feeding until 24-hrs after last dose
- Metronidazole 2g PO once[7]
Epididymitis/Epididymorchitis
- For acute epididymitis likely caused by STI
- Ceftriaxone 250 mg IM in a single dose PLUS
- Doxycycline 100 mg orally twice a day for 10 days
- For acute epididymitis most likely caused by STI and enteric organisms (MSM)
- Ceftriaxone 250 mg IM in a single dose PLUS
- Levofloxacin 500 mg orally once a day for 10 days OR
- Ofloxacin 300 mg orally twice a day for 10 days
- For acute epididymitis most likely caused by enteric organisms
- Levofloxacin 500 mg orally once daily for 10 days OR
- Ofloxacin 300 mg orally twice a day for 10 days
Treat sexual partner if possible
GC/Chlamydia Conjunctivitis
Chlamydial
- Doxycycline 100mg PO BID for 7 days OR
- Azithromycin 1g (20mg/kg) PO one time dose
- Newborn Treatment: Azithromycin 20mg/kg PO once daily x 3 days
- Disease manifests 5 days post-birth to 2 weeks (late onset)
Gonococcal
- Due to increasing resistance, CDC recommends dual therapy with Ceftriaxone and Azithromycin (even if patient is negative for Chlamydia).
- Ceftriaxone 250mg IM one dose PLUS
- Azithromycin 1g PO one dose
- Newborn Treatment:
- Prophylaxis: Erythromycin ophthalmic 0.5% x1
- Disease manifests 1st 5 days post delivery (early onset)
- Treatment Ceftriaxone 25-50mg IV or IM, max 125mg
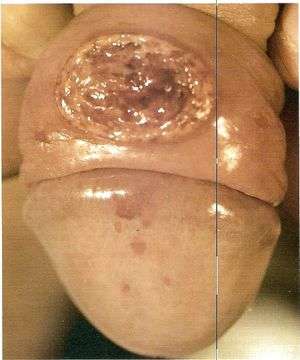
Herpes
Initial Episode[9]
- Acyclovir OR
- 400mg PO q8hrs x 7-10 days
- or 200mg PO 5x/day x 7-10 days
- Valacyclovir 1g PO q12hrs x 7-10 days OR
- Famciclovir 250mg PO q8hrs x 7-10 days
Recurrence[9]
- Acyclovir OR
- 400mg PO q8hrs x 5 days
- or 800mg PO q12hrs x 5 days
- or 800mg PO q8hrs x 2 days
- Valacyclovir OR
- 500mg PO q12hrs x 3 days
- or 1g PO qd x 5 days
- Famciclovir
- 125mg PO q12hrs for 5 days
- or 1g PO q12hrs for 1 day
- or 500mg PO once, followed by 250mg PO q12hrs for 2 days
Suppressive Therapy[9]
- Acyclovir 400mg PO q12hrs daily OR
- Famciclovir 250mg PO q12hrs daily OR
- Valacyclovir 500mg-1g PO daily (500mg may be less effective)
Lymphogranuloma Venereum
- Doxycycline 100mg PO BID x 21 days (first choice) OR
- Erythromycin 500mg PO QID x 21 days OR
- Preferred for pregnant and lactating females
- Azithromycin 1g PO weekly for 3 weeks OR
- Alternative for pregnant women - poor evidence for this treatment currently
- Tetracycline, Minocycline, or Moxifloxacin (x21 days) are also acceptable alternatives to Doxycycline
- Treat sexual partner
- Doxycycline 100mg PO BID x 7 days OR
- Azithromycin 1gm PO x1
Proctitis
Inflammation of the rectum (distal 10-12cm)
- Ceftriaxone 125mg IM x1 + Doxy 100mg po bid x 7d
PID
- No sexual activity for 2 weeks;
- Treat all partners who had sex with patient during previous 60 days prior to symptom onset
Outpatient Options
- Ceftriaxone 250mg IM (or IV)[10] x1 + doxycycline 100mg PO BID x14d +/- metronidazole 500mg PO BID x14d [11]
- Metronidazole based upon assessment of risk for anaerobes; consider in:
- Pelvic abscess
- Proven or suspected infection w/ Trichomonas or Bacterial Vaginosis
- History of gynecological instrumentation in the preceding 2-3wks
- Metronidazole based upon assessment of risk for anaerobes; consider in:
- Cefoxitin 2 g IM in a single dose and Probenecid, 1 g PO administered concurrently in a single dose[12] + Doxycycline 100 mg PO BID x 14 days +/- flagyl based on above criteria
Alternative Outpatient Options
- Ceftriaxone 250mg IM x1 + 1 g of azithromycin per week, x 2 weeks[13] +/- flagyl based on above criteria
- A single randomized controlled trial shows that azithromycin is superior to doxycycline even when compliance in taking doxycycline is excellent (98.2% vs 87.5%)[13]
Inpatient
- Cefoxitin 2gm IV q6hr OR cefotetan 2gm IV q12hr) + doxycycline PO or IV 100 mg q12hr OR
- Clindamycin 900mg IV q8h + gentamicin 2mg/kg QD OR
- Ampicillin-sulbactam 3gm IV q6hr + doxycycline 100mg IV/PO q12hr
Syphilis
Early Stage
This is classified as primary, secondary, and early latent syphilis less than one year.
Treatment Options:
- Penicillin G Benzathine 2.4 million units IM x 1
- Repeat dose after 7 days for pregnant patients and HIV infection
- Doxycycline 100mg oral twice daily for 14 days as alternative
Late Stage
Late stage is greater than one year duration, presence of gummas, or cardiovascular disease
Treatment Options:
- Penicillin G Benzathine 2.4 million units IM weekly x 3 weeks
- Doxycycline 100mg oral twice daily for 4 weeks as alternative
Neurosyphilis
There are 3 Major options with none showing greater efficacy than others:
- Penicillin G 3-4 million units IV every 4 hours x 10-14 days
- Penicillin G 24 million units continuous IV infusion x 10-14 days
- Penicillin G Procaine2.4 million units IM daily + probenecid 500mg oral every 6 hours for 10-14 days.
- Alternative:
- Ceftriaxone 2gm IV once daily for 10-14 days
- Desensitization to the penicillin allergy is still the preferred method of treatment for patients with early and late stage disease (especially during pregnancy)
Trichomonas vaginalis
Pregnant
Only treat if the patient is symptomatic and avoid breast feeding until 24-hrs after last dose
- Metronidazole 2g PO once[16]
Urethritis (male)
Treatment to cover both gonorrhea and chlamydia
Uncomplicated Infection
- Ceftriaxone 250mg IM once, PLUS
- Azithromycin 1g PO once OR
- Doxycycline 100mg PO BID x 7 days
Cephalosporin Allergy
- Azithromycin 2g PO once, PLUS
- Gentamicin 240mg IM once[18]
- In theory this high dose macrolide will provide treatment for both GC and Chlamydia
Partner treatment
- Cefixime 400mg PO once, PLUS
- Azithromycin 1g PO once, OR
- Doxycycline 100mg PO BID x 7 days
Recurrent or Persistent
Target M. genitalium
- Moxifloxacin 400 mg daily x 7 days
Consider coverage of trichomonas, among men who have sex with women
- Metronidazole 2 gm PO x 1, OR
- Tinidazole 2 gm PO x 1
See Also
- Human Papillomavirus (HPV)
- Pelvic Inflammatory Disease (PID)
- Ulcerative STDs
- Penile diagnoses
- Pelvic pain
- Expedited Partner Therapy
References
- CDC: STI Fact sheet 2013
- Workoski KA and Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recommen and Reports. 2015; 64(3):1-140.
- CDC Pregnancy BV Treatment Guidelines.cdc.gov
- 2015 CDC guidelines
- CDC: 2015 Sexually Transmitted Diseases Treatment Guidelines
- Kissinger P et al. Single-dose versus 7-day-dose metronidazole for the treatment of trichomoniasis in women: An open-label, randomised controlled trial. Lancet Infect Dis 2018 Oct 5; [e-pub].
- CDC Trichomoniasis 2015. https://www.cdc.gov/std/tg2015/trichomoniasis.htm
- CDC. Sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2010;59(No. RR-12)
- Workoski KA and Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recommen and Reports. 2015; 64(3):1-140.
- Hayes BD. Trick of the Trade: IV ceftriaxone for gonorrhea. October 9th, 2012 ALiEM. https://www.aliem.com/2012/10/trick-of-trade-iv-ceftriaxone-for/. Accessed October 23, 2018.
- Ness RB et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol 2002;186:929–37
- CDC PID Treatment http://www.cdc.gov/std/treatment/2010/pid.htm
- Savaris RF. et al. Comparing ceftriaxone plus azithromycin or doxycycline for pelvic inflammatory disease: a randomized controlled trial. Obstet Gynecol. 2007 Jul;110(1):53-60
- Mackay G. Chapter 43. Sexually Transmitted Diseases & Pelvic Infections. In:DeCherney AH, Nathan L, Laufer N, Roman AS. eds. CURRENT Diagnosis & Treatment: Obstetrics & Gynecology, 11e. New York, NY: McGraw-Hill; 2013
- Kissinger P et al. Single-dose versus 7-day-dose metronidazole for the treatment of trichomoniasis in women: An open-label, randomised controlled trial. Lancet Infect Dis 2018 Oct 5; [e-pub].
- CDC Trichomoniasis 2015. https://www.cdc.gov/std/tg2015/trichomoniasis.htm
- CDC. Sexually transmitted diseases treatment guidelines. MMWR Recomm Rep 2010;59(No. RR-12)
- CDC: 2015 Sexually Transmitted Diseases Treatment Guidelines
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.