Reexpansion pulmonary edema
Background
- Incidence may be as low as 1% or as high as 14%[1]
Risk Factors
Poorly understood, but may include:
- PTX > 30% in size
- PTX symptoms for prolonged time, >3 days
Prevention
- Consider using smaller bore chest tubes
- Other strategies include applying water seal only or attaching only a Heimlich valve without suction
Clinical Features
- Typically progresses over 2 days immediately after thoracentesis
- After 2 days, subsequent rapid improvement
Differential Diagnosis
Pulmonary Edema Types
Noncardiogenic pulmonary edema
- Negative pressure pulmonary edema
- Upper airway obstruction
- Reexpansion pulmonary edema
- Strangulation
- Neurogenic causes
- Iatrogenic fluid overload
- Multiple blood transfusions
- IV fluid
- Inhalation injury
- Pulmonary contusion
- Aspiration pneumonia and pneumonitis
- Other
- High altitude pulmonary edema
- Hypertensive emergency
- ARDS
- Sympathetic crashing acute pulmonary edema (SCAPE)
- Immersion pulmonary edema
- Hantavirus pulmonary syndrome
- Missed dialysis in kidney failure
Evaluation
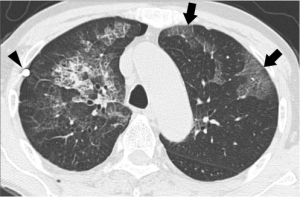
Bilateral re-expansion pulmonary edema seven hours after thoracentesis for right pneumothorax. Reveals mixed ground-glass opacity and minimal consolidation combined with intralobular reticulations and interlobular septal thickening; Note tip of chest tube (arrowhead).
- Radiographic opacities in previously collapsed lung
Management
- Supportive, as is with other forms of noncardiogenic pulmonary edema
- If a patient requires intubation, positive pressure ventilation improves symptoms after 24-48 hours
Disposition
See Also
External Links
References
- Mukhopadhyay A, Mitra M, Chakrabati S. Reexpansion pulmonary edema following thoracentesis. J Assoc Chest Physicians [serial online] 2016 [cited 2018 Oct 11];4:30-2. Available from: http://www.jacpjournal.org/text.asp?2016/4/1/30/159871.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.