Radial head fracture
This page is for adult patients; see radial head fracture (peds) for pediatric patients
Background
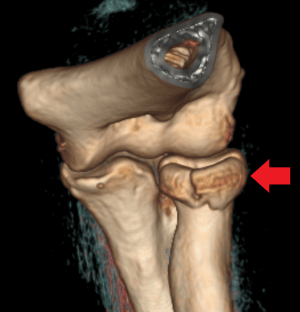
Radial head fracture seen on 3D CT reconstruction.
- Most common fractures of the elbow, approximately 20% of elbow fractures
- Caused by FOOSH in pronation leading to radial head being driven into the capitellum
Associated injuries (are common)
- Capitellum fracture
- Olecranon fracture
- Coronoid fracture
- MCL injury
- Elbow dislocation
- DRUJ (distal radial ulnar joint) injury
- Interosseous membrane disruption
- Essex-Lopresti fracture (radial head fracture, DRUJ, interosseous membrane disruption), requires ORIF
- Terrible triad (radial head fracture, coronoid fracture, elbow dislocation)
Clinical Features
- Pain in the lateral elbow, especially with pronation/supination of forearm
- Swelling laterally and tenderness of radial head
Differential Diagnosis
Radiograph-Positive
- Distal humerus fracture
- Radial head fracture
- Capitellum fracture
- Olecranon fracture
- Elbow dislocation
Radiograph-Negative
- Lateral epicondylitis
- Medial epicondylitis
- Olecranon bursitis (nonseptic)
- Septic bursitis
- Biceps tendon rupture/dislocation
Evaluation
Workup
- Elbow PA & lateral
- Consider x-rays of humerus, forearm, and wrist (e.g. to rule out a Essex-Lopresti fracture)
- Consider Greenspan (radial head-capitellum) view X-Ray
- Lateral elbow is shot at 45 degrees to pick up subtle fractures
Diagnosis
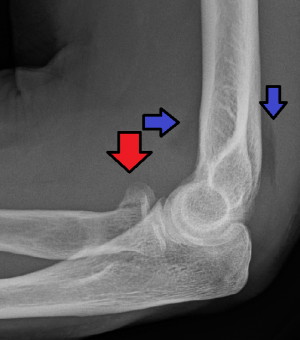
Radial head fracture (red arrow) with posterior and anterior sail signs (blue arrows)

Anterior and posterior fat pad signs (in a case of an undisplaced fracture of the radius head, which is not visible directly).
- Ensure there is no tenderness over the rest of the forearm/wrist to rule out an Essex-Lopresti fracture
- Typically diagnosed on elbow X-ray (fractures are often subtle)
- Look for abnormal fat pad
- Look for radiocapitellar line disruption
Management
General Fracture Management
- Acute pain management
- Open fractures require immediate IV antibiotics and urgent surgical washout
- Neurovascular compromise from fracture requires emergent reduction and/or orthopedic intervention
- Consider risk for compartment syndrome
- Ice, elevation
Immobilization
- Sling immobilization in flexion
- Nondisplaced fracture with no mobility restrictions: ortho follow up within 1wk
- Displaced fracture or mobility restrictions: ortho follow up within 24hr
Disposition
- Normally outpatient
References
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.