Purpura fulminans
Background
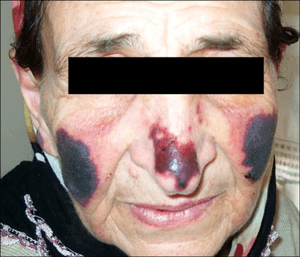
- Life-threatening syndrome of intravascular coagulation and hemmorrhagic skin infarction→ DIC and vascular collapse
- Usually occurs in children, but can occur in adults
- Most commonly in the setting of overwhelming sepsis OR 7-10 days after infection
Causes
- Meningococcus
- Streptococcus species
- Varicella
- Rickettsia sp
- Venom-induced consumptive coagulopathy (VICC) due to snake bites
- Protein C, protein S, or antithrombin III deficiency
- Drug-induced
Clinical Features
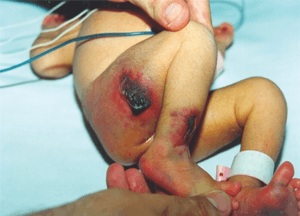
Neonatal purpura fulminans
Differential Diagnosis
Petechiae/Purpura (by findings)
- Febrile, toxic
- Palpable
- Meningococcemia
- Disseminated gonococcal infection
- Endocarditis
- Rocky mountain spotted fever
- HSP
- Non-palpable
- Purpura fulminans
- DIC
- TTP
- Palpable
- Afebrile, nontoxic
- Palpable
- Autoimmune vasculitis
- Non-palpable
- Palpable
Evaluation
- DIC work up
- CBC, PT/PTT, fibrinogen, d-dimer, FDP
- Infectious work up
Management
- Treat shock
- Treat underlying infection
- Necrotic tissue may require debridement
- Coagulopathy correction, in some cases
- Typically only if bleeding or need for procedure
- Exception: FFP usually indicated for neonatal purpura fulminans
- Cryoprecipitate: consider if fibrinogen <100
- Platelets: consider repletion if <50K with bleeding or <20K without bleeding
- FFP: consider repletion to goal of PT and PTT < 1.5 times the normal limit
- Vitamin K, folate
- Typically only if bleeding or need for procedure
Disposition
- Admit!
See Also
External Links
References
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.