Pulmonary edema
Background
Pulmonary Edema Types
Noncardiogenic pulmonary edema
- Negative pressure pulmonary edema
- Upper airway obstruction
- Reexpansion pulmonary edema
- Strangulation
- Neurogenic causes
- Iatrogenic fluid overload
- Multiple blood transfusions
- IV fluid
- Inhalation injury
- Pulmonary contusion
- Aspiration pneumonia and pneumonitis
- Other
- High altitude pulmonary edema
- Hypertensive emergency
- ARDS
- Sympathetic crashing acute pulmonary edema (SCAPE)
- Immersion pulmonary edema
- Hantavirus pulmonary syndrome
- Missed dialysis in kidney failure
Clinical Features
- Crackles
- Respiratory distress
- Increased jugular venous distension
- Signs of poor organ perfusion
Differential Diagnosis
Emergent
- Pulmonary
- Airway obstruction
- Anaphylaxis
- Angioedema
- Aspiration
- Asthma
- Cor pulmonale
- Inhalation exposure
- Noncardiogenic pulmonary edema
- Pneumonia
- Pneumocystis Pneumonia (PCP)
- Pulmonary embolism
- Pulmonary hypertension
- Tension pneumothorax
- Idiopathic pulmonary fibrosis acute exacerbation
- Cystic fibrosis exacerbation
- Cardiac
- Other Associated with Normal/↑ Respiratory Effort
- Abdominal distension
- Anemia
- CO Poisoning
- Salicylate toxicity
- Diabetic ketoacidosis (DKA)
- Diaphragm injury
- Electrolyte abnormalities
- Epiglottitis
- Flail chest
- Hypotension
- Metabolic acidosis
- Pneumonia
- Pneumothorax/hemothorax
- Renal Failure
- Sepsis
- Toxic ingestion
- Other Associated with ↓ Respiratory Effort
Pediatric-specific
- Aspirated foreign body
- Respiratory distress syndrome
- Meconium aspiration syndrome
- Bronchiolitis (peds)
- Pertussis
- Bronchopulmonary dysplasia
- Croup
- Bacterial tracheitis
- Tracheomalacia
- Congenital heart disease
- Vascular ring
- Neonatal abstinence syndrome
- Inborn errors of metabolism
- Brief resolved unexplained event
- Normal neonatal periodic breathing (misinterpreted by caregivers as abnormal)
Non-Emergent
- ALS
- Ascites
- Uncorrected ASD
- Congenital heart disease
- COPD exacerbation
- Fever
- Hyperventilation
- Interstitial lung disease
- Neoplasm
- Obesity
- Panic attack
- Pleural effusion
- Polymyositis
- Porphyria
- Pregnancy
- Rib fracture
- Spontaneous pneumothorax
- Thyroid Disease
- URI
Evaluation

Pitting pedal edema
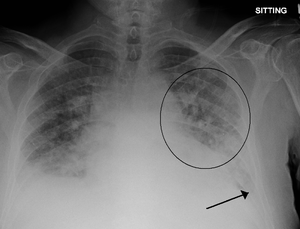
Pulmonary edema with small pleural effusions on both sides.
POCUS shows B lines[1]
- CBC (rule out anemia)
- Chem
- Albumin level
- ECG
- CXR
- Cephalization
- Interstitial edema
- Pulmonary venous congestion
- Pleural effusion
- Alveolar edema
- Cardiomegaly
- Troponin +/- BNP
- Ultrasound
- Bedside to assess global function, B lines, assessment of IVC
- Formal TTE/TEE
Brain natriuretic peptide (BNP)[2]
- Measurement
- <100 pg/mL: Negative for acute CHF (Sn 90%, NPV 89%)
- 100-500 pg/mL: Indeterminate (Consider differential diagnosis and pre-test probability)
- >500 pg/mL: Positive for acute CHF (Sp 87%, PPV 90%)
- Combination of BNP with clinician judgment 94% sensitive 70% specific (compared to 49% sn and 96% spec clinical judgement alone) [3]
Lung ultrasound of pulmonary edema
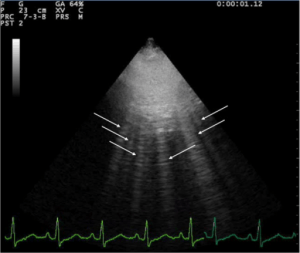
Lung ultrasound showing pulmonary edema.
- A lines and B lines
- A lines:
- Appear as horizontal lines
- Indicate dry interlobular septa.
- Predominance of A lines has 90% sensitivity, 67% specificity for pulmonary artery wedge pressure <= 13mm Hg
- A line predominance suggests that intravenous fluids may be safely given without concern for pulmonary edema
- B lines ("comets"):
- White lines from the pleura to the bottom of the screen
- Highly sensitive for pulmonary edema, but can be present at low wedge pressures
- A lines:
Management
- CPAP/BiPAP with PEEP 6-8; titrate up to PEEP of 10-12
- Nitroglycerin
- Dosing Options
- Sublingual 0.4mg q5min
- Nitropaste (better bioavailability than oral Nitroglycerin)
- Intravenous: 0.1mcg/kg/min - 5mcg/kg/min
- Generally start IV nitroglycerin 50mcg/min and titrate rapidly (150mcg/min or higher) to symptom relief as long as patient's blood pressure tolerates
- Dosing Options
- If nitroglycerin fails to reduce work of breathing, consider nitroprusside (reduces both preload and afterload) or ACE-inhibitiors (preload reducer)
- After patient improves, titrate down nitroglycerin as enalaprilat (0.625 - 1.25mg IV) or captopril are started
- Morphine is no longer recommended do to increased morbidity[7][8]
Disposition
- Depends on underlying cause, hemodynamic stability, and response to treatment
See Also
References
- http://www.thepocusatlas.com/pulmonary/
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med. 2002;347(3):161-167. doi:10.1056/NEJMoa020233.
- McCullough et al. B-Type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from breathing not properly (BNP) multinational study. Circulation. 2002:DOI: 10.1161/01.CIR.0000025242.79963.4
- Januzzi JL, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J. 2006 Feb. 27(3):330-7.
- Kragelund C, Gronning B, Kober L, Hildebrandt P, Steffensen R. N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med. 2005 Feb 17. 352(7):666-75.
- Moe GW, Howlett J, Januzzi JL, Zowall H,. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation. 2007 Jun 19. 115(24):3103-10.
- Peacock WF, Hollander JE, Diercks DB, Lopatin M, Fonarow G, Emerman CL. Morphine and outcomes in acute decompensated heart failure: an ADHERE analysis. Emerg Med J. 2008 Apr;25(4):205-9.
- Ellingsrud C, Agewall S. Morphine in the treatment of acute pulmonary oedema--Why? Int J Cardiol. 2016 Jan 1;202:870-3.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.