Proximal humerus fracture
This page is for adult patients; for pediatric patients see proximal humerus fracture (peds)
Background

- Typically occur in elderly osteoporotic patients from FOOSH mechanism
- Must rule-out axillary and brachial plexus neurovascular injuries
- 45% have nerve injury (axillary most common)
- Greater tuberosity fracture suggests rotator cuff tear
- Lesser tuberosity fracture suggests posterior shoulder dislocation
Clinical Features
- Pain, swelling, tenderness about the shoulder
- Arm is held closely against chest wall
Differential Diagnosis
Shoulder and Upper Arm Diagnoses
Traumatic/Acute:
- Shoulder Dislocation
- Clavicle fracture
- Humerus fracture
- Scapula fracture
- Acromioclavicular injury
- Glenohumeral instability
- Rotator cuff tear
- Biceps tendon rupture
- Triceps tendon rupture
- Septic joint
Nontraumatic/Chronic:
- Rotator cuff tear
- Impingement syndrome
- Calcific tendinitis
- Adhesive capsulitis
- Biceps tendinitis
- Subacromial bursitis
Refered pain & non-orthopedic causes:
- Referred pain from
- Neck
- Diaphragm (e.g. gallbladder disease)
- Brachial plexus injury
- Axillary artery thrombosis
- Thoracic outlet syndrome
- Subclavian steal syndrome
- Pancoast tumor
- Myocardial infarction
- Pneumonia
- Pulmonary embolism
Evaluation

Proximal humerus fracture
- AP, lateral, and axillary radiographs
- Fracture of articular surface suggested by pseudosubluxation:
- Superior joint hematoma pushes humerus down
- Consider CT for
- Preop surgical planning
- Greater tuberosity or humoral head position uncertain
- Intra-articular comminution
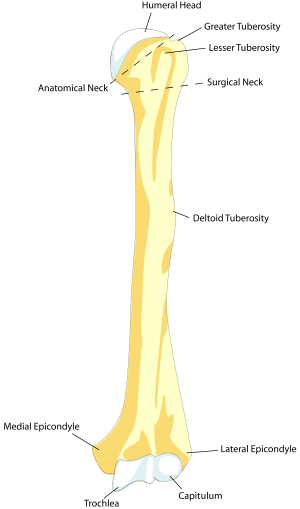
Neer System
- Proximal humerus is divided into four "parts" based on epiphyseal lines:
- Articular surface of humeral head
- Greater tubercle
- Lesser tubercle
- Shaft of humerus
- A "one-part" fracture is one in which fragment is displaced <1cm or not angulated >45deg
Management
General Fracture Management
- Acute pain management
- Open fractures require immediate IV antibiotics and urgent surgical washout
- Neurovascular compromise from fracture requires emergent reduction and/or orthopedic intervention
- Consider risk for compartment syndrome
Specific Management
- Ortho consult in the ED
- Elderly patient with comminution, multiple fractures, or poor bone might be candidates for hemiarthroplasty
- Improved outcomes if surgery within 14 days
Disposition
- Outpatient management if closed and distally neurovascularly intact
Specialty Care
Non Operative
- 85% Non-op, often with following features
- Minimally displaced
- Located at surgical neck non op if either 1 or 2 part
- Greater tuberosity fracture with < 5mm displacement
- Generally, "One-part" fracture of humeral head
- Consider in advanced age, poor bone quality, non dominant hand, co-morbid disease, other injuries
- Encourage range of motion within 14 days
Operative
- More than one-part fractures
- One part fractures of anatomical neck
- Greater than 45 degree angulation
- Greater tuberosity > 5mm displaced
- Fracture of lesser tuberosity
- "Floating" elbow, where forearm also has fracture
Complications
- Nerve injury
- Axillary nerve injury (up to 58%)
- Suprascapular nerve (up to 48%)
- Avascular Necrosis risk factors
- 4 part fractures
- Head split
- Short calcar segments
- Disrupted medial hinge
- Adhesive capsulitis
See Also
References
- Orthobullets
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.