Priapism
Background
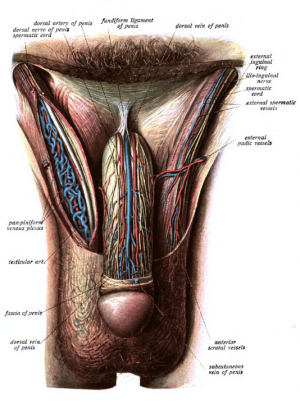
Penis anatomy
- Sustained (> 4h) erection not associated with sexual stimulation
- May lead to erectile dysfunction and penile necrosis
- High rate of sexual dysfunction if present > 24hrs
Types
High-flow (nonischemic)
- Rare
- Usually painless
- Increased arterial flow
- Usually self-resolves and does not require intervention
- Usually does not cause ischemia or sexual dysfunction
Low-flow (ischemic)
- Most common type
- Veno-occlusion causing pooling of deoxygenated blood in cavernous tissue
- Painful
- Urologic emergency
- May progress to ischemia and necrosis without intervention
Causes
- High-flow
- Arterio-cavernosal shunt due to groin or straddle injury
- High spinal injury
Clinical Features
Low-flow
- Pain
- Rigid penile shaft (corpus cavernosum)
- Flaccid penile glans and spongiosum
High-flow
- Painless
- Partially rigid shaft
- Rigid penile glans
Differential Diagnosis
- Peyronie's Disease
- Urethral foreign body
- Penile surgical implant
- Erection from sexual arousal
Evaluation
- CBC
- Consideration of leukemia or undiagnosed sickle cell disease
- Type and screen
- May require exchange transfusion in sickle cell disease
- Coagulation profile
- Consider urinalysis/toxicologic screen if unclear etiology
- Cavernosal blood gas may help differentiate high- from low-flow
- Low flow causes hypoxic, hypercarbic, and acidotic cavernosal blood gases
- pH < 7.25, pO2 < 30 mmHg, pCO2 > 60 mmHg
- Low flow causes hypoxic, hypercarbic, and acidotic cavernosal blood gases
- Ultrasound may help distinguish high- from low-flow
Management
- Pain control: Morphine and/or penile nerve block
Low Flow Priapism
Follow a step-wise approach:
- 1. Aspirate 25mL of blood from cavernosum, up to two times
- 2. Irrigate cavernosum with 25mL of cold (10°C) saline
- 3. Medication injections
Aspiration of corpus cavernosum
- Ensure procedure is appropriate
- Rarely beneficial after 48h
- Risk of impotence is high even with treatment
- Obtain consent
- Prep the area with chlorhexidine and drape appropriately
- Penile nerve block or local anesthesic at puncture site
- Insert 18 gauge needle into penile shaft at 2 and 10 o'clock positions (or 3 and 9 o'clock positions)
- Aspirate blood (usually 20 - 30 cc on each side)
- May follow with intracavernosal injections (most common is phenylephrine)
α/β-2 Agonist
- Consider terbutaline[4]
- Dose: 0.25-0.5mg SQ in deltoids OR 5-10mg PO, may repeat in q20min
- Phenylephrine
- Dilute phenylephrine 1ml of 1mg/ml in 9mL NS for final concentration of 100mcg/mL
- For 500 mcg/ml, take 0.5 ml of 10mg/ml phenylephrine, and dilute in 9.5 cc NS
- Inject base of penis with 19-Ga needle (after blood aspiration to confirm position)
- 100-200 mcg every 3-5min (max 1000 mcg) until resolution or 1 hour
- Ensure patient fully monitored, with BP, HR, pulse oximetry
- Reflex bradycardia is expected, so consider dosages relative to toleration of drop from baseline HR
- Only one side needs to be injected since there exists a vascular channel between the 2 corpora cavernosa
- Compress injection area to prevent hematoma formation
- Use with caution in cardiovascular disease
- Dilute phenylephrine 1ml of 1mg/ml in 9mL NS for final concentration of 100mcg/mL
- Epinephrine
- In pediatric population, intracavernosal injection of epinephrine instead of phenylephrine has been shown more successful in achieving detumescence
Wrap penis in elastic bandage after detumescence is achieved
High Flow Priapism
- May resolve with observation
- Consult urology for consideration of surgical correction or embolization by interventional radiology[5]
Sickle Cell Disease
- IV hydration
- Pain control
- Supplemental oxygen
- Transfusion for goal HCT>30% with consultation for partial exchange transfusion (HGB-S<30%)
- Exchange transfusion is associated with ASPEN syndrome (Association of Sickle cell Priapism, Exchange transfusion & Neurological events)
- Urology consult
Disposition
- Admit if refractory to treatment or need or IR or surgical intervention
- May discharge home if treatment is successful with close follow-up by urology
Video
START_WIDGET8af7a57c10e55814-0END_WIDGET
References
- Miller ST, Rao SP, Dunn EK, Glassberg KI. Priapism in children with sickle cell disease. J Urol. Aug 1995;154(2 Patient 2):844-7
- reen J, Hakim L. Cocaine-induced veno-occlusive priapism: importance of urine toxicology screening in the emergency room setting. Clin Urol. 1999;161
- Quan D, Ruha AM. Priapism associated with Latrodectus mactans envenomation. Am J Emerg Med. Jul 2009;27(6):759.e1-2
- Lowe FC, Jarow JP. Placebo-controlled study of oral terbutaline and pseudoephedrine in management of prostaglandin E1-induced prolonged erections. Urology. Jul 1993;42(1):51-3
- Sandro C. High-flow priapism: treatment and long-term follow-up. 2002. 59(1).110–113 PDF
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.