Myxedema coma
Background
- Hypothyroidism + mental status changes/coma + hypothermia + precipitating stressor[1]
- Majority of the patients > 60yo[2]
- Occurs in 0.1% of patients with hypothyroidism
- Usually occurs after precipitating incident in patient with untreated hypothyroidism [3]
- Mortality may be as high as 60%[4]
- Untreated mortality approaches 100% [5]
- ~50% of cases become evident after admission
- Severe hypothyroidism may be first time presentation of hypothyroid[6]
Precipitants
- Bradycardia and hypothermia
- Burns
- CHF
- CVA
- Cold exposure
- GI bleed
- Metabolic abnormalities (hypoxia, hypercapnia, hyponatremia, hypoglycemia)
- Medications: Beta blockers, sedatives, opioids, phenothiazines, amiodarone[7]
- Especially medications with CNS depressant effect [8]
- Medication non-adherence (thyroid meds)
- MI
- Sepsis
- Trauma
- PE
Spectrum of Thyroid Disease
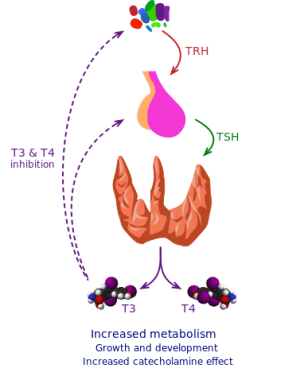
Thyroid physiology
- Myxedema coma << hypothyroidism < euthyroid > hyperthyroidism >> thyroid storm
Clinical Features

Man with myxedema or severe hypothyroidism showing an expressionless face, puffiness around the eyes and pallor.
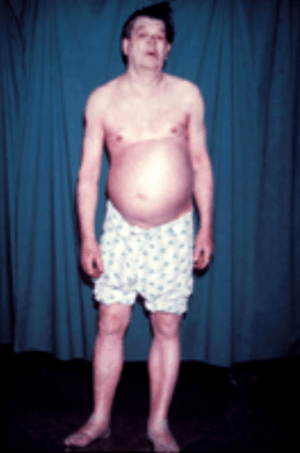
Additional symptoms include swelling of the arms and legs and ascites.

Pretibial "woody" (i.e. non-pitting) myxedema

A case of myxedema coma presenting as a brain stem infarct in a 74-year-old Korean woman. (A, B) Severe periorbital edema and thinned eyebrow. (C, D) Non-pitting edema and desquamation of the hands and feet.
Hypothermia
- Temperature <35.5°C (95.9°F).
Cardiovascular
- Bradycardia
- Hypotension
- Pericardial effusion
Pulmonary
- Hypoventilation, hypercapnia
- There is often diaphragmatic dysfunction that causes worsening hypoventilation. The dysfunction is reversed after thyroid hormone administration[9]
- Early respiratory support with intubation may be necessary to prevent respiratory collapse
- Hypoxia
- Pleural Effusion
- Upper airway obstruction from glottic edema, vocal cord edema, and macroglossia can complicate intubation.
Neurologic
- Altered mental status/Coma due to CO2 narcosis
- Coma is very rare
- Pseudomyotonic "hung up" deep tendon reflexes
- Particularly Achilles reflex
- Relaxation phase of DTR twice as long as contraction phase
- Neuropsychiatric symptoms [10]
Differential Diagnosis
Evaluation
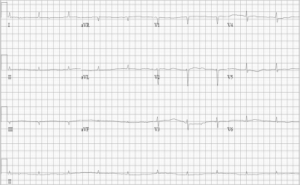
ECG showing sinus bradycardia, low QRS voltage, and a prolonged QT interval.
Work-Up
- TSH, FT4, FT3
- In primary hypothyroidism TSH will be elevated and T4 and T3 will be low
- If the patient has secondary hypothyroidism (Pituitary dysfunction) the TSH may be low or normal and T4 and T3 will be low
- Chemistry
- CBC
- Mild anemia, leukopenia
- Blood cultures
- LFTs
- Elevated transaminases
- Elevated CPK
- Cortisol level
- VBG/ABG
- Hypercapnia
- Hypoxia
- Lipid levels
- Hypercholesterolemia
- CXR
- ECG
- Sinus bradycardia
- Non-specific ST-T wave changes
- Prolonged QTc
- Ventricular dysrhythmias
- Bedside cardiac US for pericardial effusion
Diagnosis
Management
Respiratory Support
- Early mechanical ventilation will prevent respiratory collapse and severe respiratory acidosis.
Fluid Resuscitation
- Often intravascularly depleted
- May have underlying illness causing dehydration
- In patients who are hyponatremic, be cautious with rapid correction of hyponatremia
- Consider fluid restriction
- Use D5NS if hypoglycemic
- Monitor for unmasking of CHF
Hypotension
- Vasopressors will be ineffective without concomitant thyroid hormone replacement
Hormone Replacement
- Levothyroxine (T4) (generally agreed upon first line therapy)
- Dose: 100 to 500 mcg (4mcg/kg IV) followed by 75 to 100 mcg administered IV daily until the patient takes oral replacement.[11]
- Does require extrathyroidal conversion which can be reduced in myxedema but will have a slow steady onset of action
- Potentially safer in patients with CAD
- American Thyroid Association recommends treatment with both T4 and T3[12]
- T3 20mcg IV followed by 2.5-10mcg q8hr
- Start with 10mcg if elderly or has CAD
- Does not require extrathyroidal conversion
- More rapid onset but may be harmful in patients with CAD
Adrenal Insufficiency
- Hydrocortisone 100 mg IV q8h for possible concomitant adrenal insufficiency
- Alternative: dexamethasone 2-4mg q12hrs (will not affect cortisol level or ACTH stimulation test)
Hypothermia
- Treat with passive rewarming
- Hypothermia will also reverse with thyroid hormone administration
- Avoid mechanical stimulation
- Do not actively rewarm:
- Usually are volume depleted
- Rapid peripheral vasodilation may induce worsening hypotension
Disposition
- Admit to ICU
See Also
External Links
References
- Wall CR. Myxedema coma: diagnosis and treatment. Am Fam Physician. Dec 1 2000;62(11):2485-90.
- Davis PJ, Davis FB. Hypothyroidism in the elderly. Compr Ther. 1984;10:17–23.
- Thiessen, M. (2018). Thyroid and Adrenal Disorders. Rosen's Emergency Medicine (9th ed.). Philadelphia, PA: Elsevier/Saunders.
- Arlot S et al. Myxoedema coma: response of thyroid hormones with oral and intravenous high-dose L-thyroxine treatment. Intensive Care Med. 1991;17:16–8.
- Thiessen, M. (2018). Thyroid and Adrenal Disorders. Rosen's Emergency Medicine (9th ed.). Philadelphia, PA: Elsevier/Saunders.
- Nicoloff JT et al. A form of decompensated hypothyroidism. Endocrinol Metab Clin North Am. 1993;22:279–90.
- Mazonson PD et al. Myxedema coma during long-term amiodarone therapy. Am J Med. 1984;77:751–4.
- Thiessen, M. (2018). Thyroid and Adrenal Disorders. Rosen's Emergency Medicine (9th ed.). Philadelphia, PA: Elsevier/Saunders.
- Martinez FJ et al. Hypothyroidism. A reversible cause of diaphragmatic dysfunction. Chest. 1989;96:1059–63.
- Thiessen, M. (2018). Thyroid and Adrenal Disorders. Rosen's Emergency Medicine (9th ed.). Philadelphia, PA: Elsevier/Saunders.
- Smallridge RC. Metabolic and anatomic thyroid emergencies: a review. Crit Care Med. 1992;20:276–91
- Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, Celi FS, et al. Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid. 2014 Dec. 24 (12):1670-751.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.