Pneumopericardium
Background
- Air in the pericardium
- Generally secondary to connection between pericardium and pleural cavity, bronchi, or GI tract
- Most often found following trauma, severe asthma exacerbation, strangulation, or forceful drug insufflation
Causes of pneumopericardium
- GI malignancy
- PUD
- Esophageal diverticula
- Barotrauma
- Mechanical ventilation
- Vigorous bag-mask ventilation
- SCUBA diving/rapid ascent
- Drug insufflation (especially associated with crack cocaine)
- Asthma
- Valsalva
- Infection pericarditis with gas-producing bacteria
- Thoracic surgery
- Pericardial fluid drainage
- Blast injury
- Blunt or penetrating thoracic trauma
- Neonatal respiratory distress syndrome
Clinical Features
- May present with tamponade physiology depending on size
- Other features include:
- Dyspnea
- Cyanosis
- Chest pain
- Pulsus paradoxus
- Bradycardia
- Tachycardia
- May have subcutaneous emphysema
- May have succussion splash if there is also a pericardial effusion
- May have Hamman crunch
Differential Diagnosis
Thoracic Trauma
- Airway/Pulmonary
- Cardiac/Vascular
- Cardiac injury
- Blunt cardiac injury
- Penetrating cardiac injury
- Cardiac tamponade
- Traumatic aortic transection
- Cardiac injury
- Musculoskeletal
- Other
Evaluation
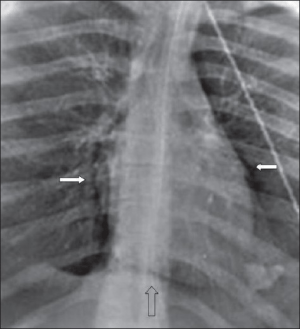
Lucent line around the heart extending up to the main pulmonary arteries (solid white arrows). Air may accumulate inferior to the cardiac shadow, which crosses the midline above the diaphragm (i.e. continuous diaphragm sign)
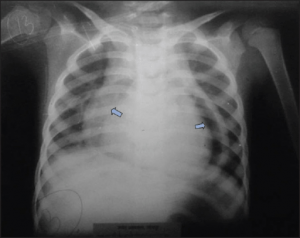
Pneumopericardium on chest x-ray after battery button ingestion.
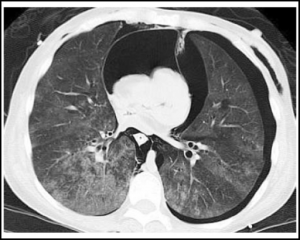
CT showing tension pneumopericardium, subcutaneous emphysema, bilateral pneumothorax, and a compressed heart.
- Assess for underlying cause
- CXR[1]
- Heart partially or completely surrounded by gas
- Pericardium sharply outlined by gas density on either side
- Continuous diaphragm sign may be present (diaphragm seen continuously across the midline
- PoCUS[2]
- Bright spots moving along pericardial layer during diastole
- Comet-tail artefacts extending across heart and disappearing during systole
Management
- Treat underlying cause
- Conservative management usually sufficient (usually self-resolves)
- If tamponade physiology, may require pericardiocentesis
- If communicating pneumothorax, chest tube placement may resolve both[3]
Disposition
- If underlying cause is stable and patient is asymptomatic, may discharge home
- Most patients will require admission for treatment of underlying cause
See Also
References
- Bell, D. et al. Pneumopericardium. Radiopaedia.org. Retrieved March 8 2019.
- Bobbia et al. (2013). Pneumopericardium diagnosis by point-of-care ultrasonography. Journal of Clinical Ultrasound, 4(14), May 2013.
- Braiteh, F., and Malik, I. (2008). Pneumopericardium. Canadian Journal of Emergency Medicine, 179(10).
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.