Pelvic inflammatory disease
Background
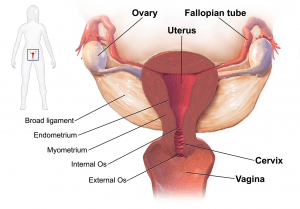
Pelvic anatomy.
- Pelvic Inflammatory Disease (PID) comprises spectrum of infections of the upper reproductive tract:
- Salpingitis, endometritis, myo/parametritis, and oophoritis
- Perihepatitis (Fitz-Hugh-Curtis) is caused by lymphatic spread
- Tubo-ovarian abscess is caused by direct extension
- It is the most common serious infection in women aged 16 to 25 years and begins as cervicitis (commonly due to GC or chlamydia) that may progress to polymicrobial infection.
- Initial lower tract infection may be asymptomatic
- Most common cause of death is rupture of a tubo-ovarian abscess
- Can be caused by organisms such as M. genitalium which is very difficult to isolate and will not be picked up on routine testing
- Bilateral tubal ligation does not confer protection against risk[1]
Clinical Features
History
- Pelvic Pain (90%)
- Vaginal discharge (75%)
- Vaginal and postcoital bleeding (>33%)
- Dysuria, fever, malaise, nausea and vomiting
Physical Exam
- Cervical motion tenderness
- Adnexal tenderness (Most sensitive finding - Sn ~95%)
- Mucopurulent cervicitis
- Absence should prompt consideration of another diagnosis
- RUQ Pain
- May indicate perihepatic inflammation (particularly if jaundice also present)
Complications
- Tubo-ovarian abscess
- Fitz-Hugh-Curtis
- Perihepatic inflammation seen only on CT, not US; LFTs are normal
- Responds to standard antibiotic regimen
- Infertility
- Ectopic pregnancy
- Chronic pelvic pain
Differential Diagnosis
Pelvic Pain
Pelvic origin
- Urinary tract infection
- Ectopic
- Ovarian torsion
- Endometriosis
- Pelvic inflammatory disease
- Cervicitis
- Ectopic pregnancy
- Ovarian torsion
- Spontaneous abortion
- Septic abortion
- Myoma (degenerating)
- Ovarian cyst (rupture)
- Tubo-ovarian abscess
- Mittelschmerz
- Sexual assault/trauma
- Ovarian hyperstimulation syndrome
Abdominal origin
Evaluation
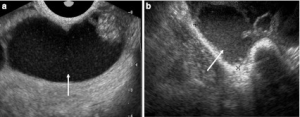
PID with pyosalpinx on transvaginal ultrasound: bilateral adenexal cysts consistent with pyosalpinges (white arrows).
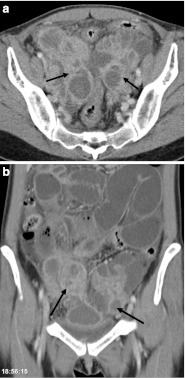
PID on CT with bilateral adnexal complex fluid-filled and thick-walled cysts typical for tubo-ovarian abcess formation and an associated ileus.
Workup
Management
- No sexual activity for 2 weeks;
- Treat all partners who had sex with patient during previous 60 days prior to symptom onset
Outpatient Options
- Ceftriaxone 250mg IM (or IV)[6] x1 + doxycycline 100mg PO BID x14d +/- metronidazole 500mg PO BID x14d [7]
- Metronidazole based upon assessment of risk for anaerobes; consider in:
- Pelvic abscess
- Proven or suspected infection w/ Trichomonas or Bacterial Vaginosis
- History of gynecological instrumentation in the preceding 2-3wks
- Metronidazole based upon assessment of risk for anaerobes; consider in:
- Cefoxitin 2 g IM in a single dose and Probenecid, 1 g PO administered concurrently in a single dose[8] + Doxycycline 100 mg PO BID x 14 days +/- flagyl based on above criteria
Alternative Outpatient Options
- Ceftriaxone 250mg IM x1 + 1 g of azithromycin per week, x 2 weeks[9] +/- flagyl based on above criteria
- A single randomized controlled trial shows that azithromycin is superior to doxycycline even when compliance in taking doxycycline is excellent (98.2% vs 87.5%)[9]
Inpatient
- Cefoxitin 2gm IV q6hr OR cefotetan 2gm IV q12hr) + doxycycline PO or IV 100 mg q12hr OR
- Clindamycin 900mg IV q8h + gentamicin 2mg/kg QD OR
- Ampicillin-sulbactam 3gm IV q6hr + doxycycline 100mg IV/PO q12hr
IUD
- No change in treatment if IUD in place (may treat without removal)
Due to inability to test for all causative pathogens and the potential for serious complications such as infertility, the CDC has made this a purposefully vague condition with a low threshold for empiric treatment
Disposition
Admit
- Tubo-ovarian abscess
- Hemodynamically unstable, TOA > 9 cm, postmenopausal, outpatient failure --> admit for surgical or VIR drainage
- Fitz-Hugh-Curtis
- Pregnancy
- Sepsis/Peritonitis
- Unable to tolerate PO
- Failed outpatient treatment
Discharge
- 72hr follow up
- Instruct patient to abstain from sex or adhere strictly to condom use until partner treatment and symptoms have abated
- HIV+ is not an automatic criteria for admission, consider overall clinical impression
See Also
- Sexually Transmitted Diseases (STD)
- Pelvic pain
References
- Shepherd SM et al. Pelvic Inflammatory Disease Clinical Presentation. Jan 2017. https://emedicine.medscape.com/article/256448-clinical#b1.
- Simms I et al. Risk factors associated with pelvic inflammatory disease. Sex Transm Infect. 2006 Dec; 82(6): 452–457.
- https://www.cdc.gov/std/tg2015/pid.htm
- Lee DC, Swaminathan AK. Sensitivity of ultrasound for the diagnosis of tubo-ovarian abscess: a case report and literature review. J Emerg Med. 2011 Feb;40(2):170-5. doi: 10.1016 PMID 20466506
- http://www.cdc.gov/std/tg2015/pid.htm
- Hayes BD. Trick of the Trade: IV ceftriaxone for gonorrhea. October 9th, 2012 ALiEM. https://www.aliem.com/2012/10/trick-of-trade-iv-ceftriaxone-for/. Accessed October 23, 2018.
- Ness RB et al. Effectiveness of inpatient and outpatient treatment strategies for women with pelvic inflammatory disease: results from the Pelvic Inflammatory Disease Evaluation and Clinical Health (PEACH) Randomized Trial. Am J Obstet Gynecol 2002;186:929–37
- CDC PID Treatment http://www.cdc.gov/std/treatment/2010/pid.htm
- Savaris RF. et al. Comparing ceftriaxone plus azithromycin or doxycycline for pelvic inflammatory disease: a randomized controlled trial. Obstet Gynecol. 2007 Jul;110(1):53-60
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.