Paronychia
Background
Nailtip Anatomy
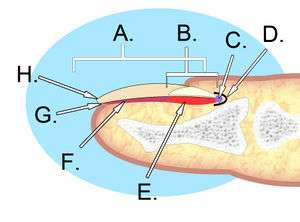
A. Nail plate; B. lunula; C. root; D. sinus; E. matrix; F. nail bed; G. hyponychium; H. free margin.
- The perinychium includes the nail, the nailbed, and the surrounding tissue.
- The paronychia is the lateral nail folds
- The hyponychium is the palmar surface skin distal to the nail.
- The lunula is that white semi-moon shaped proximal portion of the nail.
- The sterile matrix is deep to the nail, adheres to it and is distal to the lunule.
- The germinal portion is proximal to the matrix and is responsible for nail growth.
- Inflammation/infection of the proximal or lateral nail folds[1]
- Usually caused by direct or indirect minor trauma (e.g. nail-biting, manicures, hangnails, ingrown nail, dishwashing)
- Trauma allows entry of bacteria
- S. aureus is most common, although S. pyogenes, Pseudomonas pyocyanea, and Proteus vulgaris are also common[1]
Clinical Features

Paronychia of middle digit

Paronychia as a secondary infection from a splinter.
- Rapid onset of erythema, edema, and pain of proximal or lateral nail folds[1]
- Usually only affects one nail
- May see purulent drainage (expressed with pressure on nail)
Differential Diagnosis
Evaluation
- Clinical diagnosis, based on history of minor trauma and physical examination
- If unclear if wound is fluctuant:
- Have patient apply pressure to distal aspect of affected digit
- A larger than expected area of blanching, reflecting a collection of pus, may identify need for drainage
Management
Acute
- More likely to be bacterial
- If no fluctuance is identified:
- Warm compresses, soaks, elevation
- Antibiotic ointment TID x5-10 days (mild cases) ± topical steroid
- PO Antibiotics (more severe or persistent cases)[1]
- Augmentin BID x7 days OR
- Clindamycin 150-450mg TID or QID x7 days OR
- TMP-SMX DS 1-2 tab PO BID x7 days
- If fluctuance or purulence is identified:
- Consider soaking hand for preparation
- Consider digital block
- Incise area of greatest fluctuance
- Incise parallel to nail (do NOT incise perpendicular to fluctulance)
- Use iris scissors, flat tweezers, or #11 blade
- Have patient continue warm soaks at home to prevent re-accumulation
Chronic
- Multifactorial inflammation due to persistent irritation - may also have fungal component[1]
- Mainstay of therapy is avoidance of irritant
- Consider topical antifungals vs Diflucan 150mg po qweek x 4-6 weeks
- Traditional treatments have been antifungals, but accumulating evidence suggests chronic paronychia is eczematous[2]
- Topical steroids Rx to start in ED, with follow up for possible systemic steroids with PCP should be considered
- Methylprednisolone aceponate cream 0.1%, over 3 weeks
- OR betamethasone 17-valerate 0.1% for 3 weeks
Disposition
- Discharge
See Also
References
- Rigopoulos D, Larios G, Gregoriou S, Alevizos A. Acute and chronic paronychia. Am Fam Physician. 2008 Feb 1;77(3):339-46.
- Relhan V et al. Management of Chronic Paronychia. Indian J Dermatol. 2014 Jan-Feb; 59(1): 15–20.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.