Pacemaker complication
Background
Nomenclature
Paced rhythm with characteristic wide LBBB and pacer spikes

PA Xray with pacemaker
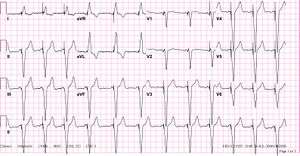
Atrial Sensed Ventricular Paced ECG

Pacer type based on Xray
| I | II | III | IV | V |
|---|---|---|---|---|
| Chamber(s) paced | Chamber(s) sensed | Response to sensing | Rate modulation | Multisite pacing |
| O = None | O = None | O = None | O = None | O = None |
| A = Atrium | A = Atrium | T = Triggered | R = Rate modulation | A = Atrium |
| V = Ventricle | V = Ventricle | I = Inhibited | V = Ventricle | |
| D = Dual (A+V) | D = Dual (A+V) | D = Dual (T+I) | D = Dual (A+V) | |
Indications
- Sinus Node Dysfunction-sinus bradycardia/arrest, sinoatrial block, chronotropic incompetence, a-fib.
- Acquired AV block- 3rd degree block and 2nd degree type II
- Chronic Bifascicular or Trifascicular block
- After Acute MI-high mortality with persistent AV block post MI
- Cardiac Resynchronization Therapy- Conduction delay (>150msec with mortality benefit) in chronic systolic heart failure further decreases EF, increases remodeling and increased MR.
- Neurocardiogenic Syncope and Carotid Sinus Syndrome
Methods to Identify Manufacturer
- Patient most often has a pocket card indicating manufacturer
- Magnet types are specific to each model so use magnets to deactivate pulse generator
- Manufactuer Hotline has patient database
- Medtronic Inc. (1-800-328-2518)
- St. Jude Medical Inc. (1-800-722-3774)
- Manufactuer code on pulse generator is visible on Chest Xray
Electromagnetic Interference
- Nonmedical
- Cell phones: do not interact with device
- Airport security: may trigger alarm, no alteration of activity
- Medical Sources
- MRI: mostly safe, consult cards on device specific recs
- Cardioversion: Use AP pads >8cm from device to minimize adverse effects
Differential Diagnosis
Pacemaker Malfunction
Problems with pocket
- Infection
- Most commonly Staphylococcus aureus or S. epidermidis
- 2% local wound infection; 1% sepsis/bacteremia
- Hematoma
- Typically occurs shortly after placement
Problems with leads
- Lead separation
- Lead dislodgment may cause thrombosis or myocardial rupture
- Lead infection can cause severe sepsis
- Leads can cause tricuspid regurg, diagnosis with TTE
- Lead coiling (ie: Twiddler's Syndrome)
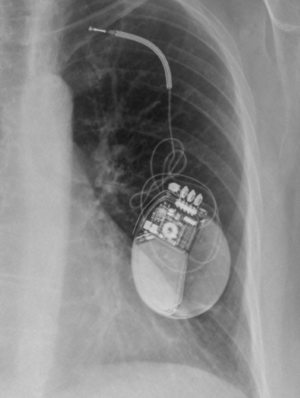 Twiddler Syndrome after large pocket and pacemaker wires spinning on themselves
Twiddler Syndrome after large pocket and pacemaker wires spinning on themselves
Failure to Capture
- Def-delivery of pacing stimulus without depolarization
- Functional- myocardium in refractory state or tissue reaction around lead insensitive
- Pathologic- drugs, myocardial disease, lytes
- Causes-lead dislodgement, fracture, perforation, insulation defect
Failure to Pace
- Def-failure to deliver a stimulus to the heart (with or with out capture)
- Oversensing-most common cause-retrograde P’s, T’s, skeletal muscle myopotentials,
- Crosstalk- type of oversensing-vent lead senses atrial pacing stim, and ventilator output inhibited
Failure to Sense
- Signal sensed when myocardial depol sent up leads and into pacemaker, if voltage exceeds threshold, pacing inhibited(appropriately)
- Most commonly break in lead/insulation, battery
- Voltages of patient's intrinsic QRS complex is too low to be detected
- New intrinsic arrhythmia, AMI, electrolyte abnormalities, lead separation, battery depletion
Runaway Pacing
- Physiologic electrical activity (T waves, muscle potentials)
- External electromagnetic interference
- Signals generated by interaction of different portions of the pacing system
- Potentially life-threatening as it can cause V-Fib or (paradoxically) bradycardia due to failure to capture
Pacemaker Mediated Tachycardia
- Also known as Endless Loop Tachycardia
- Formation of a re-entrant circuit causing inappropriate tachycardia
- Tachycardia does not exceed programmed upper limit rate on pacemaker
Evaluation
Expected ECG Patterns
- Absence of pacer artifact indicates intrinsic depolarization
- Pacing artifacts preceding depolarizations indicate successful pacing and capture
- Leads in RV apex produce LBBB pattern with appropriate discordance
- New RBBB pattern may indicate lead in LV
- Simultaneous depol of ventricles produces dominant R wave in V1
Plain Film Findings
- Obtain PA/Lateral Films to confirm pulse generator, manufacturer, lead placement/number/integrity
- R atrial lead J shaped(tip medially on AP) entering right atrial appendage
- RV leads point downward with tip between left spine and cardiac apex--lateral XR shows inferior and anterior
- Coronary sinus lead- courses posteriorly on lateral XR
- Extra leads may be appropriately abandoned and capped
- ICD component appears as thickened shock coil
Management
Disposition
- Infection - admission with MRSA coverage antibiotics, consult to cardiology, with likely replacement of pacemaker after 4-6 weeks of IV antibiotics
See Also
References
- Bernstein AD. et al. The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group. Pacing Clin Electrophysiol 2002 Feb; 25(2) 260-4. lmid:11916002
- EB Medicine- Sept 2014- Managing Pacemaker-Related Complications and Malfunctions in the Emergency Department
- Barold SS, Falkoff MD, Ong LS, Heinle RA. Pacemaker endless loop tachycardia: termination by simple techniques other than magnet application. Am J Med. 1988;85(6):817-22.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.