Otitis externa
Background
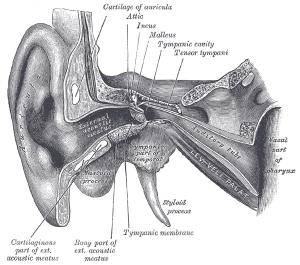
Ear anatomy
Microbiology
- Pseudomonas (most common)
- Staph/Strep
- Enterobacter
- Proteus mirabilis
- Fungus (may present after antibiotic treatment)
- Aspergillus
- Candida
Risk Factors
- Swimming
- Excessive Q-tip use
Clinical Features

Mild otitis externa

Severe otitis externa
- Rapid onset (generally within 48 hours) in the past 3 weeks, AND.[1]
- Symptoms
- otalgia (often severe)
- itching, or fullness, WITH OR WITHOUT
- hearing loss or jaw pain AND...
- Signs
- tenderness of the tragus, pinna, or both OR
- diffuse ear canal edema, erythema, or both WITH OR WITHOUT
- otorrhea
- regional lymphadenitis
- tympanic membrane erythema, or
- cellulitis of the pinna and adjacent skin
Differential Diagnosis
External
- Auricular hematoma
- Auricular perichondritis
- Cholesteatoma
- Contact dermatitis
- Ear foreign body
- Herpes zoster oticus (Ramsay Hunt syndrome)
- Malignant otitis externa
- Otitis externa
- Otomycosis
- Tympanic membrane rupture
Inner/vestibular
Evaluation
- Normally clinical
Management
Hygiene
- Clean the ear canal (Grade C)
- Cerumen wire loop or cotton swab usually works best
- 1:1 dilution of 3% hydrogen peroxide if tympanic membrane is visible and intact
- Acetic acid wash for debridement of dead skin
- Place a wick if the ear canal is fully obstructed
Prevention
- Keep ear canal dry
- Abstain from water sports for 7-10 days
Antibiotics
- Floxin otic: 5 drops in affected ear BID x 7 days[1]
- Safe with perforations
- Cipro HC otic: 3 drops in affected ear BID x 7 days
- Contains hydrocortisone to promote faster healing
- Not safe with perforation
- CiproDex: 4 drops in affected ear BID x 7 days
- Similar to Cipro HC but contains dexamethasone
- Cortisporin otic (neomycin/polymixin B/hydrocortisone)
- 4 drops in ear TID-QID x 7days
- Use suspension (NOT solution) if possiblity of perforation
- Animal studies suggest possible toxicity from the neomycin although rigorous data is lacking[2]
- Immunosuppressed (poorly controlled diabetes, chemotherapy, chronic high dose corticosteroid use, immunosuppressive drugs, neutropenia) give systemic antibiotic (ciprofloxacin or ofloxacin) [3]
Disposition
- Follow up in 1-2wks for patients with moderate disease
See Also
- Otitis Media (Peds)
- Malignant Otitis Externa
External Links
References
- Clinical Practice Guideline: Acute Otitis Externa Executive Summary. Otolaryngology -- Head and Neck Surgery 2014 150: 161 DOI: 10.1177/0194599813517659 PDF
- Wright, C. et al. Ototoxicity of neomycin and polymyxin B following middle ear application in the chinchilla and baboon. Am J Otol. 1987 Nov;8(6):495-9.
- Santos F, Selesnick SH, Gurnstein E. Diseases of the External Ear. In:Current Diagnosis and Treatment in Otolaryngology: Head and Neck Surgery, Lalwani AK (Ed), Lange Medical Books/McGraw-Hill, New York 2004.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.