Emergent delivery
Background
- 4 million deliveries per year in the US
- Highest pregnancy rates seen in 25-29 year old females[1]
Stages of Labor
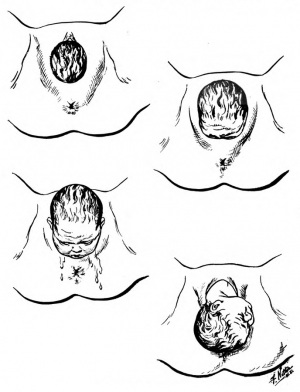
| Stage | Info | Image |
| 1st: Dilation |
|
|
| 2nd: Birth |
|
|
| 3rd: Placental delivery |
|
|
| 4th: Post-placental delivery |
|
6 Cardinal Movements of Fetal Descent[2]
- Engagement
- Flexion
- Descent
- Internal rotation
- Extension
- External rotation
Clinical Features
- Abdominal pain
- Rupture of membranes
- Pooling of fluid in the vaginal vault
- Ferning pattern when fluid is allowed to dry on microscopic slide
- pH testing with nitrazine paper turning blue
- Crowning
Differential Diagnosis
Emergent delivery and related complications
Evaluation
Stage 2: Birth
Cervical Dilatation
- Diameter of the internal cervical os increases as labor progresses
- 0 cm (closed/fingertip) to 10 cm (complete/fully dilated)
- Measure with index and middle fingers of examining hand
- Use sterile gloves, sterile lubrication, and sterile speculum
Effacement
- Assessment of the cervical thinning
- Percentage of normal 3-4 cm long cervix
- 4cm cervix = 0%
- 0cm (thin) cervix = 100%
- Fully effaced cervix feels paper-thin
Station (-5 to +5)
Distance of the presenting body relative to the maternal ischial spines
- -3 = beginning of second stage of labor
- 0 = in line with the plane of the maternal ischial spines
- +3 = impending delivery
- +4 to +5 = crowning
True versus False Labor
- False labor is defined as uterine contractions that do not produce cervical changes.
- Braxton-Hicks contractions: Brief contractions, irregular in both duration and intensity
- True labor is characterized by regular contractions that lead to cervical changes, gradually increasing in intensity and duration
Management
Preparation
- Position patient in the dorsal lithotomy position[3]
- Put on personal protective equipment
- Prepare suction, airway equipment, and warmer for infant
- Call for OB, NICU, pediatrics
- Call for additional staff members
- Divide team into maternal team and infant team (to receive infant after delivery)
Emergent Delivery Instructions (2nd Stage)
Perineal inspection
- Infant's head bulges the perineum
- If prolapsed cord is present, elevate the presenting fetal part, place patient in Trendelenburg position, and call OB stat
- Gentle digital stretching with a lubricated finger may prevent tears and lacerations
- Support the perineum with a sterile towel and place the other hand over the occiput to promote fetal head extension
Slowly deliver the head
- Check for nuchal cord
- If present, slip finger between infant's neck and cord and attempt to reduce cord by pulling over infant's head
- If unable to reduce cord, clamp or cut cord if infant's face can be cleared from perineum with immediate suction
- If present, slip finger between infant's neck and cord and attempt to reduce cord by pulling over infant's head
Deliver anterior shoulder
- Position hands on either side of the head and exert a gentle downward force[4]
Deliver posterior shoulder
- Maintain position of hands and apply a small amount of upward traction
Delivery of the body
- Controlled expulsion helps to prevent perineal lacerations
After delivery of infant
- Hold the infant securely
- Position in a manner that facilitates the flow of blood from the placenta to the infant
- Stimulate and dry the infant
- Clamp then cut the umbilical cord 3cm distal to insertion at umbilicus with sterile scissors, wait 1-3 minutes following delivery
- If uncomplicated delivery with clear airway and good respiratory support, mother may hold child immediately (skin to skin)
- If mother or infant is unstable, pass infant to receiving team
- Place infant in a warm incubator
- Check APGAR scores at 1, 5, and 10 minutes after delivery
- See newborn resuscitation for complications
Emergent Delivery Instructions (3nd Stage)
- Placental delivery
- Maintain manual suprapubic pressure
- Provide gentle cord traction and allow spontaneous placental separation
- Placenta usually delivers within 10-30 minutes
- Avoid excessive cord traction to prevent uterine inversion
- Signs of placental separation
- Abrupt lengthening of cord
- Sudden gush of blood
- Cephalad migration of uterus
- Inspect for missing placental segments and normal cord insertion and vessels
- Normal cord should have 3 vessels
- If placenta is not intact, there may be retained products of conception in the uterus requiring manual or surgical removal
- Start oxytocin 20U-40U in 1L NS at 200-500 mL/hr or give oxytocin 10U IM in a patient without IV access
- Administering oxytocin prevents 40% of PPH
Emergent Delivery Instructions (4th Stage)
- 1st hour after placental delivery
- Palpate abdomen and check for the achievement of uterine firmness and contraction
- Period of time with highest risk for postpartum hemorrhage (>500 mL blood)
Disposition
- Admit
Complications
References
- Cunningham, F., Leveno, K., Bloom, S., Spong, C., Dashe, J. Williams Obstetrics, 24th Ed. McGraw-Hill Education, 2014. Chapter 47.
- Tintinalli, Judith E., J. Stephan Stapczynski, O. John Ma, David M. Cline, Rita K. Cydulka, Garth D. Meckler, The American College of Emergency Physicians. Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 7th Ed. The McGraw-Hill Companies, Inc. 2011. Chapters 103-105.
- Marx, John MD, Hockberger, R. MD, Walls, R. MD. Rosen’s Emergency Medicine-Concepts and Clinical Practice 8th Ed. Elsevier, 2013. Chapters 34, 37, 178, 179.
- Del Portal DA et al. Emergency department management of shoulder dystocia. J Emerg Med. 2014 Mar;46(3):378-82.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.


