Mastitis
Background
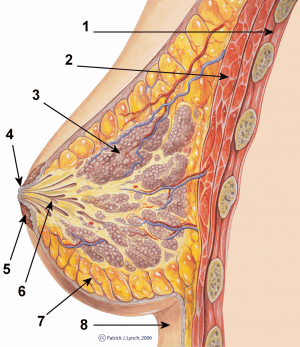
Cross-section scheme of the mammary gland: 1) Chest wall 2) Pectoralis muscles 3) Lobules 4) Nipple 5) Areola 6) Lactiferous duct 7) Adipose tissue 8) Skin
- Inflammation of the breast tissue - can be infectious or non-infectious in etiology.[1]
- Continuum of disease - Plugged ducts → engorgement → non-infectious inflammation → infectious inflammation → abscess
- Infection occurs due to bacterial colonization secondary to areolar inflammation and glandular obstruction
- Often occurs during the first few weeks to months postpartum, usually staph species with breast milk as culture medium
- Post-menopausal usually due to E. coli, Group D strep, Staph, anaerobes[2][3]
- Usually sub-areolar area due to chronic duct inflammation
- 40% recurrence rates even after I&D
- Neonatal mastitis management is controversial, but typically requires IV and/or PO antibiotics with good staph coverage
Clinical Features

Mastitis of right breast

Mastitis localized to inferior portion of left breast.
- Erythematous region on breast with well-localized area of tenderness
- Fever/chills
- Flu-like symptoms
Differential Diagnosis
Diagnostic Evaluation
Management
- If lactation mastitis, continue to breastfeed or pump, no need to dispose of breastmilk
- Warm compresses and massage, wearing supportive bra
Antibiotics
- No need to routinely interrupt breastfeeding with puerperal mastitis.
- For mild symptoms <24 hours, supportive care may be sufficient[1]
- Effective milk removal (frequent breast feeding - use pumping to augment milk removal)
- Analgesia (NSAIDs)
Treatment directed at S. aureus and Strep and E. coli
- Uncomplicated mastitis → 10 days of antibiotics (regardless of MRSA suspicion)[4]
- Dicloxacillin 500mg PO q6hrs, considered first line if breastfeeding given safety for infant OR
- Cephalexin 500mg PO q6hrs OR
- Add TMP/SMX 2DS tabs PO q12hrs if suspect MRSA
- Clindamycin 450mg PO q8hrs (also provides MRSA coverage) OR
- Amoxicillin/Clavulanate 875mg PO q12hrs OR
- Azithromycin 500mg PO x1 on day 1, then 250mg PO daily for days 2-5
Abscess
- Antibiotics as above
- If fluid collection is greater than 2cm, evacuation is recommended, with culture and sensitivity to guide antibiotic therapy
- If superficial <1cm from skin, I&D at bedside is recommended
- If deep >1cm, consider percutaneous 18g needle aspiration. Percutaneous aspiration may also be appropriate for superficial abscess in a lactating patient to avoid milk duct fistula.
- if palpable mass persists after 14-21 days, ultrasound and needle biopsy should be performed of solid components by radiology department
Disposition
- Discharge, typically
- If signs of sepsis or WBC >15K or with left shift, consider IV antibiotics and admission
- Consider referral for outpatient Specialty Breast Services:
- recurrent mastitis/abscess, or chronic granulomatous mastitis
References
- Amir LH. ABM Clinical Protocol #4: Mastitis, Revised March 2014. Breastfeeding Medicine. 2014;9(5):239-243. doi:10.1089/bfm.2014.9984.
- Eryilmaz R et al. Management of lactational breast abscesses. Breast. Oct 2005;14(5):375-9.
- Dixon JM. Outpatient treatment of non-lactational breast abscesses. Br J Surg. Jan 1992;79(1):56-7.
- Levine BL. 2011 EMRA Antibiotic Guide. EMRA. Pg 78.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.