Systemic lupus erythematosus
Background
- Autoimmune disorder affecting all systems
- Also consider drug induced lupus
Epidemiology
- Female:Male 10:1
- Peak in 20s-30s
- More common in Black patients
Clinical Features

Typical "butterfly" malar rash.
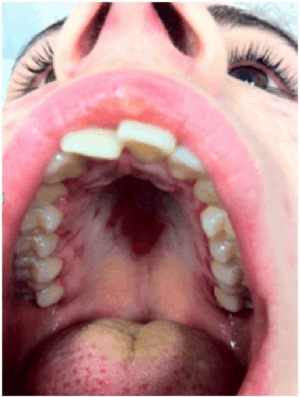
Palatal ulcer in SLE
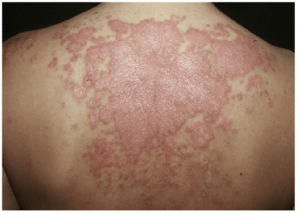
Subacute cutaneous SLE
SLICC Classification Criteria 2012 [1] Requirements: >4 of the following criteria (at least 1 clinical and 1 laboratory) OR biopsy proven lupus nephritis with positive ANA or Anti-dsDNA
- Clinical criteria
- Malar rash, bullous lupus, photosensitivity
- Discoid rash, hypertrophic lupus
- Oral ulcers or nasal ulcers
- Non-scarring alopecia
- Synovitis
- Serositis
- Nephritis
- Cerebritis, myelitis, neuropathy
- Hemolytic anemia
- Leukopenia or lymphopenia
- Thrombocytopenia
- Immunological criteria
- ANA
- Anti-dsDNA
- Anti-Sm
- Antiphospholipid antibody
- Low complement C3, low C4
- Direct Coombs' test in the absence of haemolytic anaemia
Organ system affected:
- Cardiopulmonary
- Pneumonia
- Cover for Listeria and Pseudomonas
- CAD
- More common and more complications post-PCI
- PE
- Pericarditis
- Endocarditis
- Infectious and Libman-Sachs
- Pneumonia
- Neuropsychiatric/Altered mental status
- Non-convulsive status epilepticus
- CNS vasculitis
- Stroke
- Encephalitis
- Meningitis
- Musculoskeletal
- Arthritis
- Usually symmetric
- Consider septic arthritis if there is a single inflamed joint
- Cover for Salmonella in addition to standard coverage
- Arthritis
- GI
- Lupus enteritis (mesenteric vasculitis)
- Most common cause of acute abdominal pain
- Pancreatitis
- PUD
- Lupus enteritis (mesenteric vasculitis)
- Dermatologic
- Malar rash across bridge of nose
- Discoid rash, erythematous with scale
- Renal
- Usually a nephritis
- Can cause a glomerulonephrosis
Differential Diagnosis
- Rheumatoid arthritis
- Sjögren Syndrome
- Dermatomyositis
- Polymyositis
- Stevens-Johnson syndrome
- Toxic Epidermal Necrolysis
- Septic Arthritis
- Lyme Disease
- Vasculitis
- Acute Rheumatic Fever
- Toxic Shock Syndrome
- TTP
- ITP
- DIC
Polyarthritis
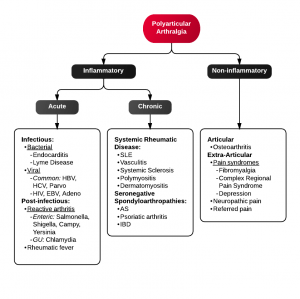
Algorithm for Polyarticular arthralgia
- Fibromyalgia
- Juvenile idiopathic arthritis
- Lyme disease
- Osteoarthritis
- Psoriatic arthritis
- Reactive poststreptococcal arthritis
- Rheumatoid arthritis
- Rheumatic fever
- Serum sickness
- Systemic lupus erythematosus
- Serum sickness–like reactions
- Viral arthritis
Causes of Glomerulonephritis
Evaluation
Undiagnosed
- CBC
- Chem 10
- Urine pregnancy
- ANA
- ESR
- Urinalysis
- Bedside echocardiography if ill or hypotensive
- (Consider anti-DNA, anti-Smith, anti-Nuclear, anti-phospholipid, C3,C4, direct Coombs')
Flare
- Bedside echo if ill or hypotensive
- CBC
- Chem
- Urinalysis
- Urine pregnancy
- As directed by organ system involved
Drug Induced Lupus
- Anti-histone-Ab positive 95% of the time
- Make sure to review medications
- High risk:
- Procainamide (antiarrhythmic)
- Hydralazine (antihypertensive)
- Moderate to low risk:
- Infliximab anti (TNF-α)
- Etanercept anti (TNF-α)
- Isoniazid (antibiotic)
- Minocycline (antibiotic)
- Pyrazinamide (antibiotic)
- Quinidine (antiarrhythmic)
- D-Penicillamine (anti-inflammatory)
- Carbamazepine (anticonvulsant)
- Oxcarbazepine (anticonvulsant)
- Phenytoin (anticonvulsant)
- Propafenone (antiarrhythmic)
- Chlorpromazine (antipsychotic)
- High risk:
Fever in SLE
- Must differentiate disease activity (flare) from infection
Risk Factors for Infection [2]
- Neutropenia/Lymphopenia
- Hypocomplementemia
- Immunosuppressive therapy (especially azathioprine [3])
Studies
Management
- Inflammatory complications
- Methylprednisolone 1-2mg/kg in most cases
- Infectious
- Stress dose steroids with hydrocortisone 100mg IV Q8hr if on or recently on steroids
- Dermatologic
- Hydrocortisone 1% cream
- If drug induced lupus, stop medication and consider alternative
Disposition
- Suspected new diagnosis can have out patient workup if well appearing
- Mild flairs can have expedited out patient management
- Musculoskeletal symptoms can usually be managed as out patients
- Chest pain requires urgent ACS evaluation
- Infections usually require admission for antibiotics and systemic corticosteroids
See Also
- Arthritis
- Fever and Rash
- Lupus Anticoagulant
- Pericarditis
- Pericardial Effusion and Tamponade
- Acute Renal Failure
- Adrenal Crisis
References
- Lisnevskaia L, et al. Systemic Lupus Erythematosus. Lancet. 2014 May 29. Epub ahead of print.
- Cuchacovich, R., & Gedalia, A. (2009). Pathophysiology and clinical spectrum of infections in systemic lupus erythematosus. Rheumatic diseases clinics of North America, 35(1), 75–93. doi:10.1016/j.rdc.2009.03.003
- Zhou, W. J., & Yang, C.-D. (2009). The causes and clinical significance of fever in systemic lupus erythematosus: a retrospective study of 487 hospitalised patients. Lupus, 18(9), 807–812. doi:10.1177/0961203309103870
- Kim, H.-A., Jeon, J.-Y., An, J.-M., Koh, B.-R., & Suh, C.-H. (2012). C-reactive protein is a more sensitive and specific marker for diagnosing bacterial infections in systemic lupus erythematosus compared to S100A8/A9 and procalcitonin. The Journal of rheumatology, 39(4), 728–734. doi:10.3899/jrheum.111044
- Scirè, C. A., Cavagna, L., Perotti, C., Bruschi, E., Caporali, R., & Montecucco, C. (2006). Diagnostic value of procalcitonin measurement in febrile patients with systemic autoimmune diseases. Clinical and experimental rheumatology, 24(2), 123–128.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.