Lower back pain
Background
- Pain lasting >6wks is risk factor for more serious disease
- Night pain and unrelenting pain are worrisome symptoms
- Back pain in IV drug user is spinal infection until proven otherwise
- 95% of herniated discs occur at L4-L5 or L5-S1 (for both pain extends below the knee)
- Lumbago: acute, nonspecific back pain
Back Pain Risk factors and probability of Fracture or Malignancy[1]
| Factor | Post Test Probability (95%CI) |
| Older Age (>65yo) | 9% (3-25%) |
| Prolonged corticosteroid | 33% (10-67%) |
| Severe trauma | 11% (8-16%) |
| Presence of contusion or abrasion | 62% (49-74%) |
| Multiple red flags | 90% (34-99%) |
| History of malignancy | 33% (22-46%) |
Clinical Features
Symptoms by Causes of Low back pain
| Musculoskeletal pain | Spinal stenosis | Sciatica | Cauda equina syndrome | Rheumatologic | |
| Radiation? | No | Possible (can be bilateral) | Yes (in the distribution of a lumbar or sacral nerve root) | Possible | ? |
| Worsened by: | Movement (e.g. twisting of torso) | Walking (pseudo-claudication) and prolonged standing | Coughing, Valsalva, sitting | Morning stiffness >30minutes | |
| Improved by: | Rest | Forward flexion, especially sitting | Lying in supine position | Movement throughout the day | |
| Other symptoms: | Urinary/bowel disturbances, perineal anaesthesia | Other rheum symptoms (e.g. ankylosing spondylitis, psoriatic arthropathy, IBD arthropathy, Reiter's disease) |
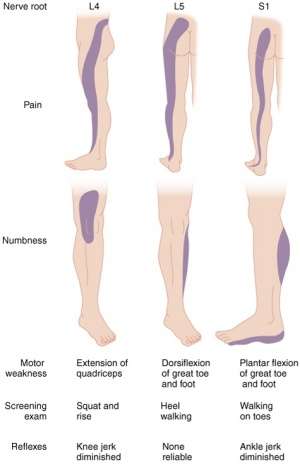
Lumbar nerve root distribution
Waddell's Signs of Non-Organic Low back pain[2]
3 or more positives suggest non-organic or alternative organic source:
- Over-reaction to the examination
- Widespread superficial tenderness not corresponding to any anatomical distribution
- Pain on axial loading of the skull or pain on rotation of the shoulders and pelvis together
- Severely limited straight leg raising on formal testing in a patient who can sit forwards with the legs extended
- Lower limb weakness or sensory loss not corresponding to a nerve root distribution
Differential Diagnosis
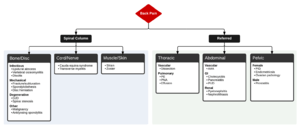
Differential diagnosis of back pain
Lower Back Pain
- Spine related
- Acute ligamentous injury
- Acute muscle strain
- Disk herniation (Sciatica)
- Degenerative joint disease
- Spondylolithesis
- Epidural compression syndromes
- Spinal fracture
- Cancer metastasis
- Spinal stenosis
- Transverse myelitis
- Vertebral osteomyelitis
- Ankylosing spondylitis
- Spondylolisthesis
- Discitis
- Renal disease
- Kidney stone
- Pyelonephritis
- Nephrolithiasis
- Intra-abdominal
- Abdominal aortic aneurysm
- Ulcer perforation
- Retrocecal appendicitis
- Large bowel obstruction
- Pancreatitis
- Pelvic disease
- PID
- Other
Evaluation
Exam
- Straight leg raise testing
- Screening exam for a herniated disk (Sn 68-80%)
- Lifting leg causes radicular pain of affected leg radiating to BELOW the knee
- Pain is worsened by ankle dorsiflexion
- Pain may be relieved by pressing across biceps femoris and pes anserinus tendons behind knee ('bowstringing')
- Crossed Straight leg raise testing (high Sp, low Sn)
- Lifting the asymptomatic leg causes radicular pain down the affected leg
- Nerve root compromise
- Rectal exam, perineal sensation, palpable bladder?
- To rule out cauda equina syndrome
Labs
- Pregnancy test
- Only necessary if concerned for infection, tumor, or rheumatologic cause
- CBC, UA, ESR (90-98% Sn for infectious etiology)
- Consider post void residual
- Can be done with non invasively with Ultrasound
Imaging
- Plain films
- Only necessary if suspect fracture, tumor, or infection
- Part of ACEP Choosing wisely
- MRI
- Only necessary if suspect infection, neoplasm, epidural compression syndromes
- Consider for back pain >6-8wks
- Ultrasound
- Rule-out AAA
Management
Acute, Non-traumatic, Non-Radicular Back Pain
- Instruct to continue daily activities using pain as limiting factor
- Medications
- Acetaminophen and/or NSAIDs
- 1st line therapy
- Consider gel/patch like diclofenac or ketoprofen (shown to be more effective than PO form and placebo in one study[3])
- Lidocaine patch
- Capsaicin or Cayenne
- Skin desensitization upon repeated exposure
- Muscle relaxants (limited evidence)
- cyclobenzaprine 10 mg PO OR
- methocarbamol 1500 mg PO
- Opioids
- Appropriate for moderate-severe pain but only for limited duration (<1 week)
- Acetaminophen and/or NSAIDs
Not Indicated
Acute, Radicular Back Pain (Sciatica)
80% of patients will ultimately improve without surgery
- Treatment is mostly the same as for acute non-radicular back pain
- Consider also gabapentin (titrate slowly) or TCAs (nortriptyline, amytriptyline)
- Gabapentin Oral: Immediate release: 400mg-1200mg PO TID
Spinal stenosis
- Treatment is the same as for musculoskeletal back pain
Cauda equina syndrome
- Immediate spine surgery consultation for spinal decompression to avoid permanent bowel/bladder/neurologic injury
Disposition
- Normally outpatient, as long as no signs of emergent pathology and able to ambulate
See Also
- Back Pain (Red Flags)
External Links
Video
START_WIDGET099a4d268f755d61-0END_WIDGET
References
- Downie A, et al. Red flags to screen for malignancy and fracture in patients with low back pain: systematic review. BMJ. 2013; 347:f7095.
- Waddell G, et al. Non-organic physical signs in low-back pain. Spine. 1980; 5:117-125.
- Mazières B, Rouanet S, Velicy J, et al. Topical ketoprofen patch (100 mg) for the treatment of ankle sprain: a randomized, double-blind, placebo-controlled study. Am J Sports Med. 2005;33:515-523
- Friedman BW, et al. "Diazepam is no better than placebo when added to Naproxen for acute low back pain." Annals of EM. August 2017. 70(2):169-176
- Holve, RL, et al. Oral steroids in initial treatment of acute sciatica. J Am Board Fam Med. 2008; 21(5):469-474.
- Goldberg H, et al. Oral steroids for acute radiculopathy due to a herniated lumbar disk: a randomized clinical trial. JAMA. 2015 May 19;313(19):1915-23. PMID 25988461.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.