Intubation
Indications
- Failure to ventilate
- Failure to oxygenate
- Inability to protect airway
- Gag reflex is absent at baseline in ~1/3 of people[1], so lack of gag reflex is inadequate in determination of ability to protect airway.
- Anticipated clinical course (anticipated deterioration, need for transport, or impending airway compromise)
- Combative patient who needs imaging (suspicion of intracranial process, etc)
Considerations
- 2015 AHA ACLS guidelines deemphasize placement of advanced airway placement in initial resuscitation
- Out-of-hospital arrest data suggests lower survival of those intubated in field[2]
- 108,000 patients examined in U.S. registry of inpatient hospital arrests, with 95% of intubations occurring within 15 min of resuscitation[3]
- Patients intubated were significantly less likely to survive to discharge, 16% vs. 19%
- Also less likely to be discharged with good functional status, 11% vs. 14%
Absolute Contraindications
- No absolute contraindications when performed as an emergent procedure
- Exception: cannot ventilate and anticipate near impossible orotracheal intubation, strongly consider surgical airway
Relative Contraindications
See Predicting the difficult airway
Difficult BVM (MOANS)
- Mask seal
- Obesity
- Aged
- No teeth
- Stiffness (resistance to ventilation)
Difficult Intubation (LEMON)
- Look externally (gestalt)
- Evaluate 3-3-2 rule
- Mallampati
- Obstruction
- Neck mobility
Equipment Needed

Normal intubation view.
- Medications
- Induction agent
- Paralytic agent
- Laryngoscope (type based on clinical indication and provider preference)
- Direct laryngoscope with blade of provider's choice or
- Video laryngoscope (Glidescope, C-Mac, KingVision, etc.) or
- Optical stylet (Shikani, Levitan, etc.) or
- Fiberoptic device
- Endotracheal tube
- End-tidal CO2 device (colorimetric or quantitative)
- Ventilator
- Suction
- Intubation adjuncts (bougie, lighted stylet, etc)
- Ensure you have correct stylet for type of laryngoscope you are using
- BVM
- OPA/NPA
- Method of preoxygenation (NC, NRB, C-PAP, etc)
- Nasal cannula for apneic oxygenation
SOAP-ME Checklist Mnemonic
- Suction
- Oxygen
- Nasal cannula
- Non-rebreather
- Bag-valve mask
- Airways
- Endotracheal tube
- Rescue devices
- Adjuncts
- Positioning
- Medications
- Equipment
- Laryngoscope
- EtCO2
- Bougie
Post-Procedure
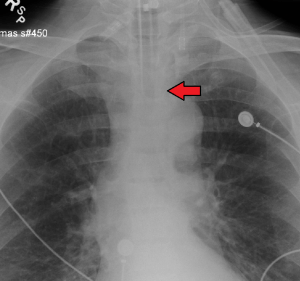
An endotracheal tube in good position on CXR. Arrow marks the tip.
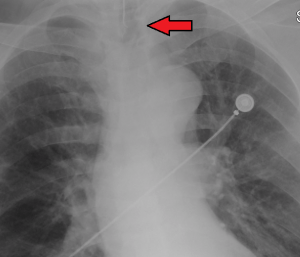
An endotracheal tube not deep enough. Arrow marks the tip.
Initial ventilation settings
| Disease | Tidal Volume (mL/kg^) | Respiratory Rate | I:E | PEEP | FiO2 |
| Traditional | 8 | 10-12 | 1:2 | 5 | 100% |
| Lung Protective (e.g. ARDS) | 6 | 12-20 | 1:2 | 2-15 | 100% |
| Obstructive (e.g. bronchoconstriction) | 6 | 5-8 | 1:4 | 0-5 | 100% |
| Hypovolemic | 8 | 10-12 | 1:2 | 0-5 | 100% |
Complications
Special Situations
Severe Metabolic Acidosis
Further drop in pH during intubation can be catastrophic
- NIV (SIMV Vt 550, FiO2 100%, Flow Rate 30 LPM, PSV 5-10, PEEP 5, RR 0)
- SIMV on ventilator, not NIV machine
- "Pseudo-SIMV" mode
- Attach end-tidal CO2 and observe value
- Push RSI medications
- Turn the respiratory rate to 12
- Perform jaw thrust
- Wait 45sec
- Intubate
- Re-attach the ventilator
- Immediately increase rate to 30
- Change Vt to 8cc/kg
- Change flow rate to 60 LPM (normal setting)
- Make sure end-tidal CO2 is at least as low as before
Active GI Bleed
- Empty the stomach
- Place an NG and suction out blood
- Varices are not a contraindication
- Metoclopramide 10mg IV
- Increases LES tone
- Place an NG and suction out blood
- Intubate with HOB at 45°
- Preoxygenate!
- Want to avoid bagging if possible
- Intubation meds
- Use sedative that is BP stable (etomidate, ketamine)
- Use paralytics (actually increases LES tone)
- If need to bag:
- Bag gently and slowly (10BPM)
- Consider placing LMA
- If patient vomits
- Place in Trendelenberg
- Place LMA
- Use meconium aspirator
- If patient aspirates anticipate a sepsis-like syndrome
- May need pressors, additional fluid (not antibiotic!)
Video
START_WIDGET17c374f91168ff88-0END_WIDGET
See Also
External Links
References
- Davies AE, Kidd D, Stone SP, MacMahon J. Pharyngeal sensation and gag reflex in healthy subjects. Lancet. 1995 Feb 25;345(8948):487-8.
- Hasegawa K et al. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA 2013 Jan 16; 309:257.
- Angus DC.Whether to intubate during cardiopulmonary resuscitation: Conventional wisdom vs big data. JAMA 2017 Feb 7; 317:477.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.