Herpes zoster ophthalmicus
Background
- Occurs when varicella zoster virus is reactivated in the ophthalmic division (V1) of trigeminal nerve
- 50% of cases associated with ocular involvement
- Highly suggested by vesicles at tip of nose (Hutchinson's sign)
- Nasociliary branch of V1 innervates both the lateral/tip of nose as well as the cornea
- Consider immunocompromise in patients <40yrs
Clinical Features
- Prodrome of headache, malaise, photophobia, fever
- Unilateral pain or hypesthesia in V1 distribution
- Hyperemic conjunctivitis, episcleritis, lid droop
- Vesicular rash in V1 distribution
- Slit-lamp exam:
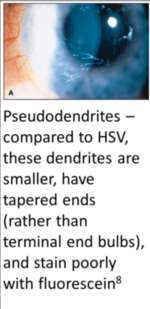
- Pseudodendrite (poorly staining mucous plaque with no epithelial erosion
- In contrast to HSV which has true dendrite with epithelial erosion and staining
- Cell and flare
- Pseudodendrite (poorly staining mucous plaque with no epithelial erosion
Differential Diagnosis
Conjunctivitis Types
Varicella zoster virus
- Varicella (Chickenpox)
- Herpes zoster (Shingles)
- Herpes zoster ophthalmicus
- Herpes zoster oticus (Ramsay Hunt syndrome)
HIV associated conditions
- HIV neurologic complications
- HIV pulmonary complications
- Pneumocystis jirovecii pneumonia (PCP)
- Tuberculosis (TB)
- CMV pneumonia
- Ophthalmologic complications
- Other
- HAART medication side effects[1]
- HAART-induced lactic acidosis
- Neuropyschiatric effects
- Hepatic toxicity
- Renal toxicity
- Steven-Johnson's
- Cytopenias
- GI symptoms
- Endocrine abnormalities
Evaluation
- Clinical
Management
- Cool compresses/lubrication drops
- Topical antibiotics to skin to prevent secondary infection
- Antiviral therapy indicated for rash <1wk duration
- Acyclovir IV 10mg/kg q8hrs x7-10 days[2] OR
- Famciclovir 500mg PO q8hrs x14 days OR
- Valacyclovir 1g PO q8hrs
- Prevention of reactivation
- Acyclovir PO 500mg 5x per day
- Ophtho consultation regarding steroid use
Disposition
- Immunocompetent patient: Oral antiviral.
- Immunocompromised patient: ”IV acyclovir and hospitalization is recommended. Neuroimaging is advised in patients with vision loss.”[3]
See Also
References
- Gutteridge, David L MD, MPH, Egan, Daniel J. MD. The HIV-Infected Adult Patient in The Emergency Department: The Changing Landscape of the Disease. Emergency Medicine Practice: An Evidence-Based Approach to Emergency Medicine. Vol 18, Num 2. Feb 2016.
- Wills Eye Manual, 6th edition
- SAEM Clinical Image Series: A Case of a Painful Facial Rash. J Chan, et al. Aliem accessed Dec 16, 2019 available online at https://www.aliem.com/2019/12/saem-clinical-image-series-facial-rash/
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.