Hematuria
This page is for adult patients; for pediatric patients see hematuria (peds)
Background
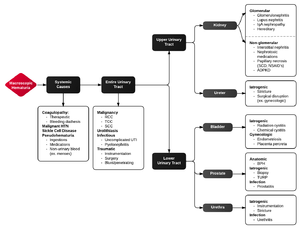
Macroscopic Hematuria algorithm
- Make sure hematuria is not myoglobin or bleeding from non-urinary source
- Hematuria + pain suggests UTI or nephrolithiasis
- Hematuria + no pain suggests malignancy, hyperplasia, or vascular cause
Common Causes
- Pediatric patients
- Glomerulonephritis
- UTI
- Congenital urinary tract anomaly
- Younger adults
- UTI
- Nephrolithiasis
- Older adults
- UTI
- Neoplasm
- BPH
- Any age
- Schistosomiasis (most common cause worldwide)
Clinical Features
Types of hematuria
- Initial hematuria
- Blood at beginning of micturition with subsequent clearing
- Suggests urethral disease
- Intervoid hematuria
- Blood between voiding only (voided urine is clear)
- Suggests lesions at distal urethra or meatus
- Total hematuria
- Blood visible throughout micturition
- Suggests disease of kidneys, ureters, or bladder
- Terminal hematuria
- Blood seen at end of micturition after initial voiding of clear urine
- Suggests disease at bladder neck or prostatic urethra
- Gross hematuria
- Indicates lower tract cause
- Microscopic hematuria
- Tends to occur with kidney disease
- Brown urine with RBC casts and proteinuria
- Suggests glomerular source
- Clotted blood
- Indicates source below kidneys
Workup
- Labs:
- Urinalysis
- Microscopic hematuria associated with proteinuria suggests glomerular disease and requires further investigation (as an outpatient)
- Urinalysis
- Consider CT imaging to assess for renal tumors, stones, or aneurysm
- Ultrasound useful to assess for hydronephrosis or a Abdominal Aortic Aneurysm
Blunt Trauma[1]
Renal injuries are associated with:
- Sudden deceleration injury without hematuria
- Gross Hematuria
- Microscopic Hematuria with Shock (SBP<90 mm Hg)
- The degree of hematuria does not correlate with significance of renal injury
Differential Diagnosis
Hematuria
- Urologic (lower tract)
- Any location
- Ureter(s)
- Dilatation of stricture
- Bladder
- Transitional cell carcinoma
- Vascular lesions or malformations
- Chemical or radiation cystitis
- Prostate
- Benign prostatic hypertrophy
- Prostatitis
- Urethra
- Stricture
- Diverticulosis
- Foreign body
- Endometriosis (cyclic hematuria with menstrual pain)
- Renal (upper tract)
- Glomerular
- Glomerulonephritis
- IgA nephropathy (Berger disease)
- Lupus nephritis
- Hereditary nephritis (Alport syndrome)
- Toxemia of pregnancy
- Serum sickness
- Erythema multiforme
- Nonglomerular
- Interstitial nephritis
- Pyelonephritis
- Papillary necrosis: sickle cell disease, diabetes, NSAID use
- Vascular: arteriovenous malformations, emboli, aortocaval fistula
- Malignancy
- Polycystic kidney disease
- Medullary sponge disease
- Tuberculosis
- Renal trauma
- Glomerular
- Hematologic
- Primary coagulopathy (e.g., hemophilia)
- Pharmacologic anticoagulation
- Sickle cell disease
- Myoglobinuria - positive blood, no RBCs: rhabdomyolysis
- Hemoglobinuria - positive blood, no RBCs
- TTP / HUS
- DIC
- Mechanical valve emergency
- Hemolytic anemia
- Paroxysmal Nocturnal Hemoglobinuria
- Miscellaneous
- Eroding abdominal aortic aneurysm
- Malignant hypertension
- Loin pain–hematuria syndrome
- Renal vein thrombosis
- Exercise-induced hematuria
- Cantharidin (Spanish fly) poisoning
- Stings/bites by insects/reptiles having venom with anticoagulant properties
- Schistosomiasis
- Sickle Cell Trait
Pediatric Hematuria
| Macroscopic Hematuria | Transient Microhematuria | Persistent Microhematuria |
| Blunt abdominal trauma | Strenuous exercise | Benign familial hematuria |
| Urinary tract infection | Congenital anomalies | Idiopathic hypercalciuria |
| Nephrolithiasis | Trauma | Immunoglobulin A nephropathy |
| Infections | Menstruation | |
| Poststreptococcal glomerulonephritis | Bladder catheterization | Alport syndrome |
| High fever | Sickle cell trait or anemia | |
| Immunoglobulin A nephropathy | Henoch-Schonlein purpura | |
| Hypercalciuria | Drugs and toxins | |
| Sickle cell disease | Lupus nephritis |
Management
- Treat underlying cause
- Gross hematuria
- Often associated with intravesicular clot formation and bladder outlet obstruction
- Use triple-lumen urinary drainage catheter with intermittent or continuous bladder irrigation
- Adequate urinary drainage must be ensured; otherwise consult urology
- Use triple-lumen urinary drainage catheter with intermittent or continuous bladder irrigation
- Often associated with intravesicular clot formation and bladder outlet obstruction
Disposition
- Outpatient management appropriate if:
- Hemodynamically stable without life-threatening cause of hematuria
- Able to tolerate oral fluids, antibiotics, and analgesics as indicated
- No significant anemia or acute renal insufficiency
- Patients <40 yr: refer to primary care provider for repeat UA within 2wk
- Patients >40 yr with risk factor for urologic cancer: refer to urologist within 2wk
- Risk factors:
- Smoking history
- Occupational exposure to chemicals or dyes
- History of gross hematuria
- Previous urologic history
- History of recurrent UTI
- Analgesic abuse
- History of pelvic irradiation
- Cyclophosphamide use
- Pregnancy
- Known malignancy
- Sickle cell disease
- Proteinuria
- Renal insufficiency
- Risk factors:
- Admit:
- Intractable pain
- Intolerance of oral fluids and medications
- Bladder outlet obstruction
- Suspected or newly diagnosed glomerulonephritis
- High risk of developing complications (pulmonary edema, volume overload, hypertensive emergency)
- Pregnant women (hematuria can accompany preeclampsia, pyelonephritis or obstructing nephrolithiasis)
See Also
References
- Mee S. et al. Radiographic assessment of renal trauma: A 10-year prospective study of patient selection. J Urology. 1989 May;141(5):1095-8
Video
START_WIDGETb9b32778ac3b46ab-0END_WIDGET
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.