Gram positive bacteria
Interpretation of Key Phrases
- “Gram positive cocci in clusters” may suggest Staphyloccocus species.
- "Gram positive cocci in pairs and chains" may suggest Streptococcus species or Enterococcus species
- “Branching Gram positive rods, modified acid fast stain positive” may suggest Nocardia or Streptomyces species
Cocci
Clusters (Staph Species)
- Coagulase Positive: Staph aureus
- Always consider as true bacteremia (and not a contaminant) due to the danger of delaying treatment[1]
- Coagulase Negative:
- Staph epidermidis
- Staph saprophyticus
- UTIs in women
- Staph lugdunensis
- Rare cause of endocarditis, meningitis, and Skin and Soft Tissue Infections
- Staphylococus lugdunensis should raise concerns for endocarditis with a single positive blood culture[4]
- Staph haemolyticus
- Rare cause of endocarditis, meningitis
Chains or Pairs (Strep Species and Related)
- Enterococcus (e.g. Enterococcus faecalis, Enterococcus faecium)
- May cause bacteremia in the proper clinical setting (UTI, intra-abdominal infections, infected vascular catheters, and endocarditis)[5]
- Strep viridans
- In general are low virulence pathogens and likely contaminants (21-50% of positive blood cultures are clinically significant)
- Risk factors for VGS bacteremia include: neutropenia, oral mucositis, irradiation to the oral cavity, antibiotic prophylaxis with trimethoprim-sulfamethoxazole and fluoroquinolones, intravenous hyperalimentation, high dose chemotherapy
- Streptococcus pneumoniae (Pairs)
- Asociated with pneumonia, meningitis, peritonitis and other severe infections
- Isolation of this organism is always significant and should be treated[6]
- Other Strep Species
- ß-hemolytic streptococcus (Group A Streptococcus, Group B Streptococcus, etc)
Rods (Bacilli)
| Organism | Cult | Morphology | |
|
Small |
Aero |
tumbling | |
| Diphtheroids |
Small | Anaero |
pallisades |
| Actinomyces |
Small | Anaero |
Branching |
| Propionibac |
Small | Anaero |
clumps/pleo |
| Lactobacillus |
Variable | Both |
may chain |
| Clostridium |
Large | Anaero |
Spores |
| Bacillus | Large | Aero | Spores |
Antibiogram
| Category | Organism | Strep. Group A, B, C, G | Strep. Pneumoniae | Viridans strep | Strep. anginosus gp | Enterococcus faecalis | Enterococcus faecium | MSSA | MRSA | CA-MRSA | Staph. Epidermidis | C. jeikeium | L. monocytogenes |
| Penicillins | Penicillin G | S | S | I | S | S | I | R | R | R | R | R | S |
| Penicillin V | S | S | I | S | S | I | R | R | R | R | R | R | |
| Anti-Staphylocccal Penicillins | Methicillin | S | S | I | S | R | R | S | R | R | S | R | R |
| Nafcillin/Oxacillin | S | S | I | S | R | R | S | R | R | S | R | R | |
| Cloxacillin/Diclox. | S | S | I | S | R | R | S | R | R | S | R | R | |
| Amino-Penicillins | AMP/Amox | S | S | I | S | S | I | R | R | R | R | R | S |
| Amox-Clav | S | S | I | S | S | S | S | R | R | R | R | X2 | |
| AMP-Sulb | S | S | I | S | S | S | S | R | R | R | R | S | |
| Anti-Pseudomonal Penicillins | Ticarcillin | S | S | I | S | I | I | R | R | R | I | R | S |
| Ticar-Clav | S | S | I | S | I | I | S | R | R | I | R | X2 | |
| Pip-Tazo | S | S | I | S | S | I | S | R | R | S | X1 | X2 | |
| Piperacillin | S | S | I | S | S | I | R | R | R | R | R | S | |
| Carbapenems | Doripenem | S | S | S | S | I | R | S | R | R | S | X1 | S |
| Ertapenem | S | S | S | S | R | R | S | R | R | S | R | I | |
| Imipenem | S | S | S | S | S | I | S | R | R | S | R | S | |
| Meropenem | S | S | S | S | I | R | S | R | R | S | X1 | S | |
| Aztreonam | R | R | R | R | R | R | R | R | R | R | R | R | |
| Fluroquinolones | Ciprofloxacin | I | I | R | R | U | R | S | R | I | S | R | S |
| Ofloxacin | I | I | R | R | U | R | S | R | X1 | S | R | R | |
| Pefloxacin | R | R | X1 | X1 | R | R | S | R | X1 | S | X1 | R | |
| Levofloxacin | S | S | S | S | S | R | S | R | I | S | X1 | S | |
| Moxifloxacin | S | S | S | S | S | I | S | I | I | S | X1 | S | |
| Gemifloxacin | S | S | S | S | S | I | S | I | I | S | X1 | S | |
| Gatifloxacin | S | S | S | S | S | I | S | I | I | S | X1 | S | |
| 1st G Cephalo | Cefazolin | S | S | S | X1 | R | X1 | S | R | R | I | R | R |
| 2nd G. Cephalo | Cefotetan | S | S | S | X1 | R | X1 | S | R | R | I | R | R |
| Cefoxitin | S | S | S | X1 | R | X1 | S | R | R | I | R | R | |
| Cefuroxime | S | S | S | X1 | R | X1 | S | R | R | I | R | R | |
| 3rd/4th G. Cephalo | Cefotaxime | S | S | S | X1 | R | X1 | S | R | R | I | R | R |
| Cefizoxime | S | S | S | X1 | R | X1 | S | R | R | I | R | R | |
| CefTRIAXone | S | S | S | X1 | R | X1 | S | R | R | I | R | R | |
| Ceftaroline | S | S | S | X1 | S | X1 | S | S | S | S | X1 | X1 | |
| CefTAZidime | S | S | I | X1 | R | X1 | I | R | R | I | R | R | |
| Cefepime | S | S | S | X1 | R | X1 | S | R | R | I | X1 | R | |
| Oral 1st G. Cephalo | Cefadroxil | S | S | S | X1 | R | X1 | S | R | R | I | R | R |
| Cephalexin | S | S | S | X1 | R | X1 | S | R | R | I | R | R | |
| Oral 2nd G. Cephalo | Cefaclor/Loracarbef | S | S | S | X1 | R | X1 | S | R | R | I | R | R |
| Cefproxil | S | S | R | X1 | R | X1 | S | R | R | I | R | R | |
| Cefuroxime axetil | S | S | S | X1 | R | X1 | S | R | R | I | R | R | |
| Oral 3rd G. Cephalo | Cefixime | S | S | S | X1 | R | X1 | R | R | R | R | R | R |
| Ceftibuten | S | I | R | X1 | R | X1 | R | R | R | R | R | R | |
| Cefpodox/Cefdinir/Cefditoren | S | S | S | X1 | R | X1 | S | R | R | I | X1 | R | |
| Aminoglycosides | Gentamicin | R | R | X1 | X1 | S | S | S | R | X1 | I | R | S |
| Tobramycin | R | R | X1 | X1 | S | R | S | R | X1 | I | R | S | |
| Amikacin | R | R | X1 | X1 | S | R | S | R | X1 | I | R | S | |
| Chloramphenicol | S | S | X1 | X1 | I | I | I | R | X1 | R | R | S | |
| Clindamycin | S | S | X1 | X1 | R | R | S | R | I | R | R | X1 | |
| Macrolides | Erythromycin | I | I | X1 | X1 | R | R | I | R | I | I | R | S |
| Azithromycin | I | I | X1 | X1 | R | R | S | R | I | R | R | S | |
| Clarithromycin | I | I | X1 | X1 | R | R | S | R | I | R | R | S | |
| Ketolide | Telithromycin | S | S | X1 | X1 | I | R | S | R | I | R | R | S |
| Tetracyclines | Doxycycline | I | S | X1 | X1 | R | R | I | I | S | R | R | S |
| Minocycline | S | S | X1 | X1 | R | R | S | I | S | R | R | S | |
| Glycylcycline | Tigecycline | S | S | X1 | X1 | S | S | S | S | S | S | S | S |
| Daptomycin | S | X23 | X1 | X1 | S | S | S | S | S | S | S | I | |
| Glyco/Lipoclycopeptides | Vancomycin | S | S | X1 | X1 | S | I | S | S | S | S | S | S |
| Teicoplanin | S | S | X1 | X1 | S | I | S | S | S | I | S | S | |
| Telavancin | S | S | X1 | X1 | S | S | S | S | S | S | S | S | |
| Fusidic Acid | I | I | X1 | X1 | S | X1 | S | S | S | S | S | X1 | |
| Trimethoprim | S | I | X1 | X1 | S | R | I | I | S | S | R | S | |
| TMP-SMX | X22 | S | X1 | X1 | X22 | R | S | S | S | I | R | S | |
| Urinary Agents | Nitrofurantoin | S | S | X1 | X1 | S | S | S | S | S | X1 | R | X1 |
| Fosfomycin | X1 | S | X1 | X1 | S | I | S | S | S | X1 | X1 | R | |
| Other | Rifampin | S | S | X1 | X1 | I | R | S | S | S | S | S | S |
| Metronidazole | R | R | X1 | X1 | R | R | R | R | R | R | R | R | |
| Quinupristin dalfoppristin | S | S | X1 | X1 | R | S | S | S | S | S | S | S | |
| Linezolid | S | S | X1 | X1 | S | S | S | S | S | S | S | S | |
| Colistimethate | R | R | X1 | X1 | R | R | R | R | R | R | R | R |
Clinical Identification Chart
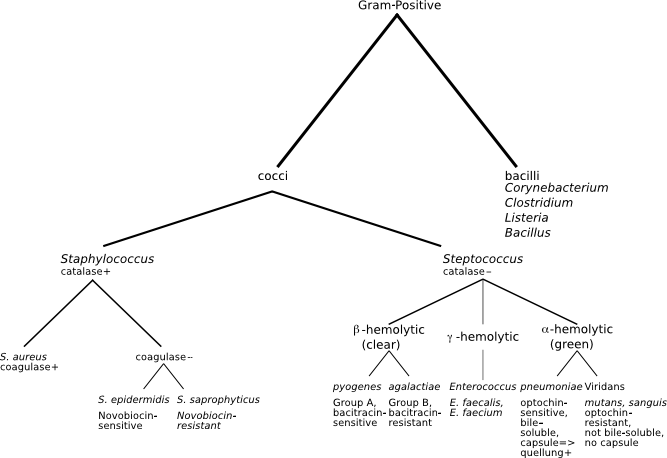
Table Overview
See Also
- Microbiology (Main)
- Bacteremia Versus Contaminated Blood Cultures
References
- Antibiotic Therapy for Positive Blood Cultures. Perez-Jorge EV, et al. Antimicrobe. http://www.antimicrobe.org/new/e38rev2.asp
- Antibiotic Therapy for Positive Blood Cultures. Perez-Jorge EV, et al. Antimicrobe. http://www.antimicrobe.org/new/e38rev2.asp
- Antibiotic Therapy for Positive Blood Cultures. Perez-Jorge EV, et al. Antimicrobe. http://www.antimicrobe.org/new/e38rev2.asp
- Liu Po-Yen et al. Staphylococcus lugdunensis Infective Endocarditis: A Literature Review and Analysis of Risk Factors. Journal of Microbiology, Immunology and Infection Volume 43, Issue 6, December 2010, Pages 478-484.
- Antibiotic Therapy for Positive Blood Cultures. Perez-Jorge EV, et al. Antimicrobe. http://www.antimicrobe.org/new/e38rev2.asp
- Antibiotic Therapy for Positive Blood Cultures. Perez-Jorge EV, et al. Antimicrobe. http://www.antimicrobe.org/new/e38rev2.asp
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.