Fifth metatarsal fracture
Background
- Os peroneum is an accessory bone (ossicle) located at the lateral side of the tarsal cuboid, proximal to the base of 5th metatarsal, commonly mistaken for a fracture
Clinical Features
Dancer or tuberosity (styloid) avulsion fracture
- Most common fracture at base of 5th metatarsal
- Sx often mild, patients usually present with sprained ankle complaint
- Occurs due to forced inversion foot/ankle while in plantar flexion
Jones or metaphyseal-diaphyseal junction fracture
- Second most common fracture at base of 5th metatarsal
- Abrupt onset of lateral foot pain, with no prior history of pain at that site, suggests acute injury and helps distinguish from stress injury
- Occurs due to sudden change in direction with heel off the ground
- Edema & ecchymosis usually present, may not be able to bear weight
Diaphyseal stress fracture
- Occurs through repetitive microtrauma, usually in younger athletes
- Important to identify given propensity for delayed union and nonunion
- Usually present with history of months of pain, which is more intense during exercise or weight-bearing
- always ask about persistent pain prior to acute event to help distinguish worsening stress fracture from acute fracture
Differential Diagnosis
Evaluation
Workup
- Plain radiographs are usually adequate
Diagnosis
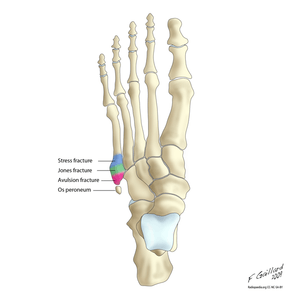
5th Metatarsal fracture types
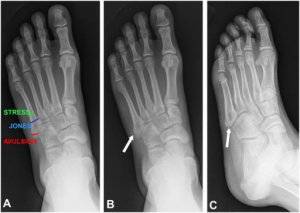
Fractures of the fifth metatarsal base. Frontal radiograph (A) demonstrates fifth metatarsal base fractures based on location. Frontal radiograph (B) in a 24-year-old runner following inversion injury demonstrates an avulsion fracture of the fifth metatarsal base. Oblique radiograph (C) in an 11-year-old boy demonstrates an unfused fifth metatarsal base apophysis, a common fracture mimic.

Jones fracture. Transverse fracture 2 cm from the base of the fifth metatarsal
- Must distinguish Jones fracture from diaphyseal stress freacture:
- Acute fracture will have narrow fracture line that appears sharp, normal thin cortex adjacent to fracture, and normal intramedullary canal
- Stress fracture will demonstrate cortical thickening near fracture line, older stress fracture will demonstrate widened fracture line and intramedullary sclerosis
Management & Disposition
General Fracture Management
- Acute pain management
- Open fractures require immediate IV antibiotics and urgent surgical washout
- Neurovascular compromise from fracture requires emergent reduction and/or orthopedic intervention
- Consider risk for compartment syndrome
Tuberosity (Styloid) Avulsion Fracture (Dancer’s or pseudo-Jones fracture)
Proximal to the more diaphyseal Jones fracture
- Refer to ortho if > 3mm displacement
- Nondisplaced fracture usually require only symptomatic treatment, RICE
- Walking boot (casting rarely necessary) and weight-bearing as tolerated, follow up in 1 week
Jones Fracture (non-displaced)
- Posterior Ankle Splint, strict NWB, RICE, ortho follow up in 3-5 days
- 50% of Jones fracture treated conservatively may result in nonunion or re-fracture
- Conservative treatment failure usually due to poor vascular supply of bone and premature return to weight-bearing
Diaphyseal Stress Fracture
- Strict NWB short-leg cast, RICE
- Ortho referral for all stress fractures
Traumatic Diaphyseal Fracture
- Posterior Ankle Splint, NWB, RICE, ortho/podiatry follow up in 3-5 days
- Dorsal or Plantar displacement >10% or 3-4mm may require reduction in ED or at referral clinic while lateral/medial displacement usually heal well without reduction
See Also
Video
START_WIDGET078dada6e9b5161a-0END_WIDGET
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.