Ewing sarcoma
Background[1]
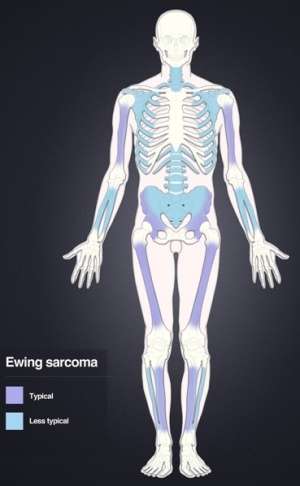
Distribution of Ewing's sarcoma: Most frequent locations are the large long bones and the pelvis.
- Highly aggressive malignant bone or soft tissue tumor arising from cells of the neuroectoderm
- One-fourth of patients will have metastasis at the time of presentation
- It is assumed that almost all patients have subclinical metastasis
- Presence and location of metastasis is the major prognostic factor for survival
- Metastasis is most frequently seen in bone (spine most common) and lungs
- Around 70 to 80 percent survival in those with non-metastatic disease
- More common in males
Clinical Features
- Constant pain for months over site of malignancy
- Worse with exercise and at night
- Site will be edematous and tender to palpation
- Mass can sometimes be appreciated
- Most often found in pelvis, axial skeleton, or diaphysis of femur with a small minority arising in soft tissues
- Pelvic tumors are more regularly associated with metastatic disease
- Fever, weight loss, fatigue, night sweats occur in less than 20 percent of patients
- Pathological fractures can occur
Differential Diagnosis
Malignant
- Multiple myeloma
- Chondrosarcoma
- Paget disease
- Osteosarcoma
- Adamantinoma
- Chordoma
- Primary bone lymphoma
- Fibrosarcoma
- Myosarcoma
Benign
- Giant cell tumor
- Chrondroblastoma
- Enchondroma
- Langerhans cell histiocytosis of bone
- Osteoblastoma
- Osteochondroma
- Osteoid osteoma
Evaluation

X-ray of a child with Ewing's sarcoma of the tibia

MRI showing Ewing's sarcoma of the left hip (white area)
- Appearance on plain radiographs often described as “onion peel” or “moth-eaten” appearance referring to the respective periosteal bone formation and osseous destruction
- LDH is a prognostic factor
- Definitive diagnosis is made with biopsy
- Work-up often includes PET scan for metastatic disease
- t(11;22) translocation is often seen
Management
- Pain control
- Neoadjuvant and adjuvant chemotherapy
- Surgery and/or radiation therapy for local control of disease
Disposition
- Home with outpatient follow up
- Admission if necessary for pain control or significant disease burden
References
- Niederhuber, John E., et al. “Sarcomas.” Abeloff's Clinical Oncology E-Book. Elsevier Health Sciences, 2019, pp. 1604 – 1654.e8.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.