Epididymitis
Background
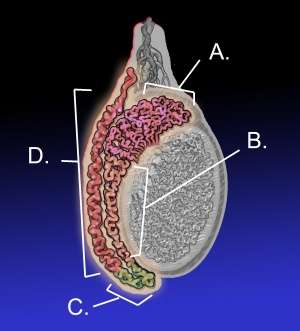
Adult testicle with epididymis (left is posterior): A. Head of epididymis, B. Body of epididymis, C. Tail of epididymis, and D. Vas deferens.
- Often confused with testicular torsion
- Cremasteric reflex intact in epididymitis
- Sexually active men <35yo → consider chlamydia, gonorrhea
- Not sexually active, age >35yo, or anal intercourse → also consider E. coli, pseudomonas, enterobacter, TB, syphilis
- Chemical epididymitis
- Consider in the patient with afib and testicular pain
- Testicular pain and swelling in patients on amiodarone
Clinical Features
Differential Diagnosis
Evaluation
Workup
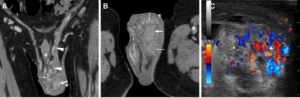
Acute epididymo-orchitis. Contrast-enhanced CT (a, b) shows thickened and engorged left spermatic cord, with inhomogeneous vascularisation of the ipsilateral epididymis (thin arrows) and testis (arrows). Ultrasound (c) reveals hypervascularisation of the epididymis (+).
Diagnosis
- Based on clinical exam or ultrasound
Management
- Scrotal elevation
- Analgesia
Antibiotics
- For acute epididymitis likely caused by STI
- Ceftriaxone 250 mg IM in a single dose PLUS
- Doxycycline 100 mg orally twice a day for 10 days
- For acute epididymitis most likely caused by STI and enteric organisms (MSM)
- Ceftriaxone 250 mg IM in a single dose PLUS
- Levofloxacin 500 mg orally once a day for 10 days OR
- Ofloxacin 300 mg orally twice a day for 10 days
- For acute epididymitis most likely caused by enteric organisms
- Levofloxacin 500 mg orally once daily for 10 days OR
- Ofloxacin 300 mg orally twice a day for 10 days
Treat sexual partner if possible
- If med adherence is an issue:
- Ceftriaxone 250mg IM once AND
- Azithromycin 1 g PO once
Pediatric Epididymitis[1]
- Rule out testicular torsion
- Bed rest to ensure lymphatic drainage
- Ice packs, acetaminophen, ibuprofen
- Rarely oral narcotics
- Pediatric urology follow up outpatient in non-toxic child for possible GU anatomical abnormalities
- Antibiotics for 10-14 days, with urine culture sent:
- Trimethroprim-sulfamethoxazole
- Amoxicillin-clavulanate
- Coverage for chlamydia and N. gonorrhoeae in suspected cases of sexual transmission
- Avoid fluoroquinolones in pediatric patients
- Severely ill or septic children:
- First generation cephalosporin AND Aminoglycoside
Disposition
- Admit for systemic signs (fever, chills, nausea/vomiting) or toxic appearance
- Discharge with urology follow-up in 1 week if non-toxic
References
- Richman MN and Bukowski TP. Pediatric Epididymitis: Pathophysiology, Diagnosis, and Management. Infect Urol. 2001;14(2).
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.