Ectopic pregnancy
Background
- Leading cause of maternal death in first trimester and overall third leading cause of maternal death
- Occur in 2% of all pregnancies[1] and as high as 6-16% in those presenting to the ED[2]
- Pregnancy in patient with prior tubal ligation or IUD in place is ectopic until proven otherwise (25-50% are ectopic)
- Even if an IUP is visualized, there is a small risk of heterotopic ectopic pregnancy
- General Population = 1 per 4000
- IVF Population = 1 per 100
Risk Factors[3][4]
Risk factors absent in almost half of patients
| Risk Factor | Odds Ratio |
| Previous tubal surgery | 21 |
| Previous ectopic pregnancy | 8.3 |
| Diethylstilbestrol exposure | 5.6 |
| Previous PID | 2.4 to 3.7 |
| Assisted Fertility | 2 to 2.5 |
| Smoker | 2.3 |
| Previous intrauterine device use | 1.6 |
Specific Types by Location
Cervical Ectopic
- Very rare with delayed diagnoses due to decreased accuracy of US
- As high as 10% with reproductive IVF
Interstitial Ectopic
- Typically presents after 8 wks, with rupture possibly occurring as early as 5 wks
- Implantation in myometrium in proximal part of fallopian tube, commonly misdiagnosed on ultrasound as intrauterine pregnancy
- 65% diagnosis on ultrasound and laparascopy is gold standard
- US characteristics:
- Empty uterus
- Gestational sac separate from endometrium
- Gestational sac > 1 cm from lateral aspect of uterine cavity
- < 5 mm mantle surrounding the sac
Clinical Features
Must consider in all women of childbearing age with abdominal and/or pelvic pain
- Ruptured
- Shock
- Rebound tenderness
- Non-ruptured (early)
- Abdominal/pelvic pain
- Vaginal bleeding
Differential Diagnosis
Vaginal Bleeding in Pregnancy (<20wks)
- Ectopic pregnancy
- Subchorionic hematoma
- First Trimester Abortion
- Complete Abortion
- Incomplete Abortion
- Inevitable Abortion
- Missed Abortion
- Septic abortion
- Threatened Abortion
- Gestational trophoblastic disease
- Consider when pregnancy-induced hypertension is seen before 24 wks of gestation
- Heterotopic pregnancy
- Implantation bleeding
- Molar pregnancy
- Non-pregnancy related bleeding
- Cervicitis
- Fibroids
- Implantation bleeding
Pelvic Pain
Pelvic origin
- Urinary tract infection
- Ectopic
- Ovarian torsion
- Endometriosis
- Pelvic inflammatory disease
- Cervicitis
- Ectopic pregnancy
- Ovarian torsion
- Spontaneous abortion
- Septic abortion
- Myoma (degenerating)
- Ovarian cyst (rupture)
- Tubo-ovarian abscess
- Mittelschmerz
- Sexual assault/trauma
- Ovarian hyperstimulation syndrome
Abdominal origin
Evaluation
Ultrasound shows ectopic pregnancy[5]
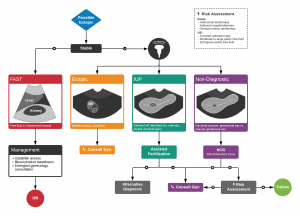
Algorithm for the Evaluation of Suspected Ectopic Pregnancy
Work-Up
Diagnostic Algorithm
Using this algorithm should always favor considering ectopic if there is any evolution or change in a patient's clinical exam[7]
| Clinical Signs and Symptoms | Risk Group | Percent Risk of Ectopic (%) |
| Peritoneal irritation or cervical motion tenderness | High | 29 |
| No fetal heart tones; no tissue at cervical os; pain present | Intermediate | 7 |
| Fetal heart tones or tissue at cervical os; no pain | <1 |
Step one
- Assess for Shock
- Beware that paradoxical bradycardia can be present with significant hemoperitoneum[9]
- If patient is a high risk for ectopic based on above estimation then immediately contact OBGYN
Step Two
Perform a Pelvic US
- Consider Transabdominal Ultrasound for B-HCG: >6000 mIU/ml (but if negative or indeterminate must do Pelvic ultrasound regardless of B-HCG)
Is there an Intrauterine Pregnancy?
Step Three
- If HCG above Discriminatory Zone (>1,500-3,000 mIU/ml) and not visualized it should be an ectopic pregnancy until proven otherwise
Step Four
- Arrange close follow-up for patients with no visualized IUP and B-HCG( (<1,500-3,000 mIU/ml), with minimal to no pain and hemodynamically stable.
- Patients should have a 48hr repeat B-HCG level checked to determine if appropriate doubling is occurring.
Repeat B-hCG Levels
| Pregnancy Type | B-hCG Change |
| Normal | Increase >53% in 48hrs (until 10,000 mIU/ml)
(This increase depends on the initial value. <1500 --> 50% inc, 1500-3000 --> 40% inc, > 3000 --> 30% inc) |
| Ectopic | Increases or decreases slowly ("plateau")^ |
| Miscarriage | Decreases >20% in 48 hrs |
^Initial level CANNOT be used to rule-out ectopic
Management
- RhoGAM for all Rh-negative women
- OB/GYN Consult
- Medical management with methotrexate (ACOG)
- Single dose regimen[12]
- Methotrexate 50mg/m2 IM day 1
- If hCG decreases by <15% between days 4 and 7, another 50mg/m2 IM methotrexate on day 7
- Absolute contraindications
- Breast-feeding
- Laboratory evidence of immunodeficiency
- Preexisting blood dyscrasias (bone marrow hypoplasia, leukopenia, thrombocytopenia, or clinically significant anemia)
- Known sensitivity to methotrexate
- Active pulmonary disease
- Peptic ulcer disease
- Hepatic, renal, or hematologic dysfunction
- Alcoholism
- Alcoholic or other chronic liver disease
- Coexistant viable IUP
- Does not have timely access to medical institution, or unwilling/unable to comply with post-MTX monitoring
- Relative contraindications
- Adnexal mass >3.5 cm in largest diameter
- Presence of fetal heart rate
- Free fluid visualized in Pouch of Douglas
- Beta-HCG >5000mIU/mL
- Note: Need to counsel patient to return after 4 and 7 days to recheck hCG values to check for satisfactory decline
- Also note that 30-60% of women experience "separation pain" ~1 week after starting methotrexate[13]
- Thought to be due to tubal distention from tubal abortion or hematoma formation
- Nevertheless, presentation of abdominal pain at this time still warrants an US to look for tubal rupture, which may be indicated by increase in pelvic free fluid, decrease in Hb
- Size of ectopic mass may actually increase before involution, and this is not associated with treatment failure
- Single dose regimen[12]
- Surgical treatment
- Urgent laparotomy if patient is unstable
- Otherwise, laparascopic salpingectomy or salpingostomy can be done
Disposition
- Most are admitted and/or go to the OR
- Smaller, minimally symptomatic ectopic pregnancies being treated with methotrexate may be discharged in consultation with OB/GYN
See Also
External Links
References
- Centers for Disease Control and Prevention. Current trends ectopic pregnancy - United States, 1990-92. MMWR Morb Mortal Wkly Rep. 1995; 44:46-48.
- Houry D and Keadey M. Complications in pregnancy part I: Early pregnancy. EBM. 2007; 9(6):1-28.
- Ankum WM, Mol BW, Van der Veen F, Bossuyt PM. Risk factors for ectopic pregnancy: a meta-analysis. Fertil Steril. 1996;65:1093–9
- Mol BW, Ankum WM, Bossuyt PM, Van der Veen F. Contraception and the risk of ectopic pregnancy: a meta-analysis. Contraception. 1995;52:337–41.
- http://www.thepocusatlas.com/obgyn/
- Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician. 2005;72;1707-1714, 1719-1720
- American College of Obstetricians and Gynecologists. Medical management of tubal pregnancy. Number 3, December 1998. Clinical management guidelines for obstetricians-gynecologists. Int J Gynaecol Obstet. 1999;65:97–103
- Buckley RG, King K et. al. History and physical examination to estimate the risk of ectopic pregnancy: validation of a clinical prediction model. Ann Emerg Med. 1999;34:589–94
- Hick JL, et al. Vital signs fail to correlate with hemoperitoneum from ruptured ectopic pregnancy. The American Journal of Emergency Medicine. 2001; 19(6)488–491.
- Mukul LV, Teal SB. Current management of ectopic pregnancy. Obstet Gynecol Clin N Am. 2007; 34:403-419.
- Yeh HC, Goodman JD, Carr L, et al. Intradecidual sign: a ultrasound criterion of early intrauterine pregnancy. Radiology. 1986;161:463-467
- Bachman EA and Barnhart K. Medical Management of Ectopic Pregnancy: A Comparison of Regimens. Clin Obstet Gynecol. 2012 Jun; 55(2): 440–447.
- Lipscomb GH et al. Management of separation pain after single-dose methotrexate therapy for ectopic pregnancy. Obstet Gynecol. 1999 Apr;93(4):590-3.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.