Ethanol toxicity
Background
- Rate of ETOH elimination is 15-30mg/dL/hr (depending on degree of chronic alcohol intake)
Clinical Features
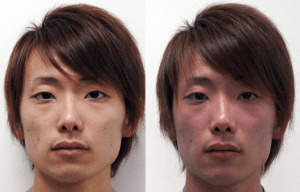
Alcohol flushing reaction: before (left) and after (right) drinking alcohol.
Classic Features
- Diminished fine motor control
- Impaired judgement and coordination
- Slurred speech
- Nystagmus
- Ataxia
- Nausea and vomiting
- Alcohol odor on breath
- Respiratory depression
- Lethargy
- Coma
Other Features (if malnourished)
Mellanby effect
- Impairment is greater at a given blood alcohol concentration when the level is rising than when it is falling. [1]
Differential Diagnosis
Ethanol related disease processes
- Ethanol toxicity
- Alcohol use disorder
- Alcohol withdrawal
- Alcohol withdrawal seizures
- Delerium tremens
- Electrolyte/acid-base disorder
Diffuse brain dysfunction
- Hypoxic encephalopathy
- Acute toxic-metabolic encephalopathy (Delirium)
- Hypoglycemia
- Hyperosmolar state (e.g., hyperglycemia)
- Electrolyte Abnormalities (hypernatremia or hyponatremia, hypercalcemia)
- Organ system failure
- Hepatic Encephalopathy
- Uremia/Renal Failure
- Endocrine (Addison's disease, Cushing syndrome, hypothyroidism, myxedema coma, thyroid storm)
- Hypoxia
- CO2 narcosis
- Hypertensive Encephalopathy
- Toxins
- TTP / Thrombotic thrombocytopenic purpura
- Alcohol withdrawal
- Drug reactions (NMS, Serotonin Syndrome)
- Environmental causes
- Deficiency state
- Wernicke encephalopathy
- Subacute Combined Degeneration of Spinal Cord (B12 deficiency)
- Vitamin D Deficiency
- Zinc Deficiency
- Sepsis
- Osmotic demyelination syndrome (central pontine myelinolysis)
- Limbic encephalitis
Primary CNS disease or trauma
- Direct CNS trauma
- Diffuse axonal injury
- Subdural/epidural hematoma
- Vascular disease
- SAH
- Stroke
- Hemispheric, brainstem
- CNS infections
- Neoplasms
- Paraneoplastic Limbic encephalitis
- Malignant Meningitis
- Pancreatic Insulinoma
- Seizures
- Nonconvulsive status epilepticus
- Postictal state
- Dementia
- Alzheimer's
- Lewy Body Dementia
- Frontotemporal Dementia
Evaluation
Clinical diagnosis. No specific workup required when there is clear evidence of alcohol intake, but the following may be considered based on clinical picture/gestalt:
- Fingerstick glucose (recommended as minimum workup in all patients with AMS)
- Consider blood alcohol level (BAL) when a good history cannot be obtained or patient fails to improve as expected
- Correlates poorly with degree of intoxication[2]
- Maintain low threshold for imaging in intoxicated patient with signs of trauma
Management
- Supportive care is mainstay of ED treatment and is based on clinical presentation
- Manage ABCs
- Benzodiazepines or haloperidol for agitation
- IV fluids are commonly used but do not hasten ETOH elimination or reduce length of stay[3][4]
Vitamin Prophylaxis for Chronic alcoholics
- At risk for thiamine deficiency, but no symptoms: thiamine 100mg PO q day
- Give multivitamin PO; patient at risk for other vitamin deficiencies
Banana bag
The majority of chronic alcoholics do NOT require a banana bag[5][6]
- Thiamine 100mg IV
- Folate 1mg IV (cheaper PO)
- Multivitamin 1 tab IV (cheaper PO)
- Magnesium sulfate 2mg IV
- Normal saline as needed for hydration
Disposition
- Caution should be taken when BAL is measured on arrival as clinical exam cannot be used alone for discharge
- Can be discharged once patient at baseline mental status, able to tolerate PO and ambulate without assistance
See Also
References
- Wang MQ, Nicholson ME, Mahoney BS, et al. Proprioceptive responses under rising and falling BACs: a test of the Mellanby effect. Percept Mot Skills. 1993 Aug;77(1):83-8.
- Olson KN, Smith SW, Kloss JS, et al. Relationship between blood alcohol concentration and observable symptoms of intoxication in patients presenting to an emergency department. Alcohol Alcohol. 2013 Jul-Aug;48(4):386-9. doi: 10.1093/alcalc/agt042.
- Perez SR, Keijzers G, Steele M. Intravenous 0.9% sodium chloride therapy does not reduce length of stay of alcohol-intoxicated patients in the emergency department: a randomised controlled trial. Emerg Med Australas. 2013 Dec;25(6):527-34. doi: 10.1111/1742-6723.12151.
- Li J, Mills T, Erato R. Intravenous saline has no effect on blood ethanol clearance. J Emerg Med. 1999 Jan-Feb;17(1):1-5.
- Krishel, S, et al. Intravenous Vitamins for Alcoholics in the Emergency Department: A Review. The Journal of Emergency Medicine. 1998; 16(3):419–424.
- Li, SF, et al. Vitamin deficiencies in acutely intoxicated patients in the ED. The American Journal of Emergency Medicine. 2008; 26(7):792–795.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.