Drug rash with eosinophilia and systemic symptoms syndrome
Background
- Known as DRESS syndrome
- A severe adverse drug reaction
- Usually begins within 8 weeks of starting a new drug
- 8-10% mortality
- Previously known as Dilantin Hypersensitivity Syndrome or Anti-convulsant hypersensitivity syndrome
- However, many other medications, particularly antibiotics
- A virus-drug interaction with HHV-6, HHV-7, EBV, and CMV may be a form of pathogenesis as well[1]
Associated Drugs
- Most common
- Phenytoin
- Phenobarbital
- Carbamazepine
- Allopurinol
- Sulfa drugs
- Others
- NSAIDS
- Anti-retrovirals
- ACE inhibitors
- Calcium-channel blockers
- Atypical antipsychotics (ziprasidone, olanzapine, etc.)[2]
- Other antibiotics
Clinical Features

DRESS induced by chloral hydrate: (A) Generalized edematous features & systemic morbilliform rash (B) Sternostomy wounds (C) hepatosplenomegaly.
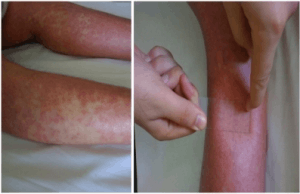
Allopurinol causing DRESS: Rash spreading symmetrically to the lower extremities (non-blanching).

DRESS due to anti-TB medication.
- Fever and rash (varying; may resemble SJS) are typically first signs
- Usually urticarial, maculopapular eruption
- In some cases vesicles, bullae, pustules, purpura, target lesions, facial edema, cheilitis, erythroderma
- +/- lymphadenopathy
- Systemic involvement may manifest as hepatitis, pneumonitis, myocarditis, pericarditis, nephritis, colitis
- Atypical lymphocytes, thrombocytopenia, neutropenia, anemia
- Leukocytosis with eosinophilia in 50-90%, and mononucleosis in 40%[3][4]
Differential Diagnosis
Erythematous rash
- Positive Nikolsky’s sign
- Febrile
- Staphylococcal scalded skin syndrome (children)
- Toxic epidermal necrolysis/SJS (adults)
- Afebrile
- Febrile
- Negative Nikolsky’s sign
Evaluation
Workup
- CBC with diff
- BMP
- LFTs
- Coags
- ESR
- CRP
- Viral hepatitis panel
- Biopsy
Diagnosis
Table of Severe Drug Rashes
| Charateristic | DRESS | SJS/TEN | AGEP | Erythroderma |
| Image |  |  |  | _Skin_Syndrome_-_Feet_Collage.jpg) |
| Onset of eruption | 2-6 weeks | 1-3 weeks | 48 hours | 1-3 weeks |
| Duration of eruption (weeks) | Several | 1-3 | <1 | Several |
| Fever | +++ | +++ | +++ | +++ |
| Mucocutaneous features | Facial edema, morbilliform eruption, pustules, exfoliative dermattiis, tense bullae, possible target lesions | Bullae, atypical target lesions, mucocutaneous erosions | Facial edema, pustules, tense bullae, possible target lesions, possibl emucosal involvement | Erythematous plaques and edema affecting >90% of total skin surface with or without diffuse exfoliation |
| Lymph node enlargement | +++ | - | + | + |
| Neutrophils | Elevated | Decreased | Very elevated | Elevated |
| Eosinophils | Very elevated | No change | Elevated | Elevated |
| Atypical lymphocytes | + | - | - | + |
| Hepatitis | +++ | ++ | ++ | - |
| Other organ involvement | Interstitial nephritis, pneumonitis, myocarditis, and thydoiditis | Tubular nephritis and tracheobronical necrosis | Possible | Possible |
| Histological pattern of skin | Perivascular lymphocytcic infiltrate | Epidermal necrosis | Subcorneal pustules | Nonspecific, unless reflecting Sezary syndrome or other lymphoma |
| Lymph node histology | Lymphoid hyperplasia | - | - | No, unless reflecting Sezary syndrome or other malignancy |
| Mortality (%) | 10 | 5-35 | 5 | 5-15 |
Management
- Discontinue suspected drug
- Supportive care: antipyretic, anti-pruritic
- Fluid management as in burn
- Systemic steroids and/or cyclosporin/immunosuppressants in severe cases (controversial)
- Hepatitis, pneumonitis, extensive exfoliative dermatitis
- Other severe systemic manifestations
- Family counseling as possible genetic component
Disposition
- Admit
See Also
References
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) Syndrome. Sonal Choudhary, Michael McLeod, Daniele Torchia, Paolo Romanelli. J Clin Aesthet Dermatol. 2013 Jun; 6(6): 31–37.
- Herman AO. Antipsychotic Linked to Potentially Fatal Skin Reaction. Physician's First Watch. Dec 12, 2014. http://www.jwatch.org/fw109630/2014/12/12/antipsychotic-linked-potentially-fatal-skin-reaction?query=pfw&jwd=000013530619&jspc=.
- Callot V, Roujeau JC, Bagot M, et al. Drug-induced pseudolymphoma and hypersensitivity syndrome. Two different clinical entities. Arch Dermatol. 1996;132:1315–1321.
- Peyriere H, Dereure O, Breton H, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2006;155:422–428.
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.