Diplopia
Background
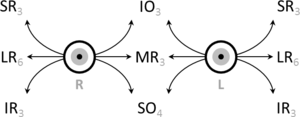
Eye movements by extra-ocular muscles and cranial nerve innervation
Monocular Diplopia
- Double vision that persists when one eye is closed
- Related to intrinsic eye problem[1]
Binocular Diplopia
- Double vision that resolves when the other eye is closed
- Related to a problem with visual axis alignment[2]
3 Main Causes Binocular Diplopia
- Eye musculature dysfunction
- Cranial nerve dysfunction
- Brainstem or intracranial process
Clinical Features
Exam
- Determine monocular vs binocular
- Evaluate for visual field defects
- Evaluate visual acuity
- Assess cranial nerves
- Multiple cranial nerve involvement suggests an intracranial process or cavernous sinus involvement
- Check extraocular muscle function
- Entrapment will show extraocular muscle restriction with extremes of gaze
- Sudden painful or non painful onset suggest a vascular cause such as thrombosis, dissection, ischemia, or vasculitis
- Other neuro deficits should raise suspicion for a CVA or MS
- Systemic illness is more likely with meningitis involving the brainstem
- Bilateral symptoms are more likely with neuromuscular problems such as Miller Fischer syndrome, botulism, or myasthenia gravis
Differential Diagnosis
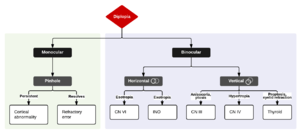
Algorithm for the Evaluation of Diplopia
Monocular Diplopia
- Cataract
- Lens dislocation
- Macular disruption
Binocular Diplopia
- Basilar Artery Thrombosis
- Posterior communicating artery (PCOM) aneurysm
- Vertebral artery dissection
- Myasthenia Gravis[3]
- Lambert-Eaton Syndrome
- Botulism
- Cavernous sinus thrombosis
- Intracranial mass, brainstem mass
- Miller Fischer variant Guillain-Barre[4]
- MS
- Hyperthyroid Proptosis
- Basilar Meningitis
- CVA
- Muscular Entrapment from Trauma
- Third nerve palsy
Evaluation
Monocular
- Slit Lamp Exam
- Assess for Cataract
- Lens symmetry
- Posterior orbital mass
- Macular dysruption
- Consider ophthalmology consult
- Consider ocular ultrasound
Binocular
- Third nerve palsy: eye is down and out
- Always needs CTH/CTA to rule out [[Posterior Communicating Artery (PCOM) Aneurysm|aneurysm given that nerve runs under PCA
- Fourth nerve palsy: head tilt down and away from side of lesion
- These are tough to catch and can be referred to ophtho outpatient for prisms
- No imaging needed unless other deficits present
- Sixth nerve palsy: eye can't track laterally
- Children need imaging to r/o tumor
- In > 50, m/l ischemic and can get MRI outpt or just watch, assuming no papilledema as it can cause isolated CN VI palsy
- If other nerves/deficits noted, consider MRI and further wu
- Other potential studies also include:
- CTH with and without contrast ± CTA neck to rule out dissection and intracranial mass
- MRV or CTV to eval for cavernous sinus thrombosis
- CT orbits w/ contrast to eval for orbital apex syndrome (like CST above, but with CN II involvement)
- MRI + DWI to if concern for CVA
- MRI ± MRA if unable to classify intracranial process on initial contrast CT with contrast
- MRI if concerned for MS
- LP if concern for meningitis
- Metabolic workup to rule out diabetes or cause of mononeuropathy
Management
Disposition
- Depends greatly on the cause of the diplopia
- Admit if:
- CVA
- Guillain-Barre
- Botulism
- ICH
- Meningitis
- Intracranial Mass with edema or shift
- Aneurysm causing compression
- Multiple cranial nerve involvement
- Isolated Cranial Nerve III and VI palsy can be discharge if close neurology follow-up and cause due to diabetes, microvascular ischemia and intracranial process ruled out[5]
See Also
External Links
References
- Coffeen P, Guyton DL: Monocular diplopia accompanying ordinary refractive errors. Am J Ophthalmol 1988; 105:451
- Rucker JC, Tomsak RL: Binocular diplopia. A practical approach. Neurologist 2005; 11:98-110
- Kusner LL, Puwanant A, Kaminski HJ: Ocular myasthenia: Diagnosis, treatment, and pathogenesis. Neurologist 2006; 12:231-239
- Bushra JS: Miller Fisher syndrome: An uncommon acute neuropathy. J Emerg Med 2000; 18:427-430
- Sanders SK, Kawasaki A, Purvin VA: Long-term prognosis in patients with vasculopathic sixth nerve palsy. Am J Ophthalmol 2002; 134:81-84
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.