Deep venous thrombosis
Background
Clinical Spectrum of Venous thromboembolism
- Deep venous thrombosis (uncomplicated)
- Phlegmasia alba dolens
- Phlegmasia cerulea dolens
- Venous gangrene
- Pulmonary embolism
- Isolated distal deep venous thrombosis
Only 40% of ambulatory ED patients with PE have concomitant DVT[1][2]
Leg Vein Anatomy
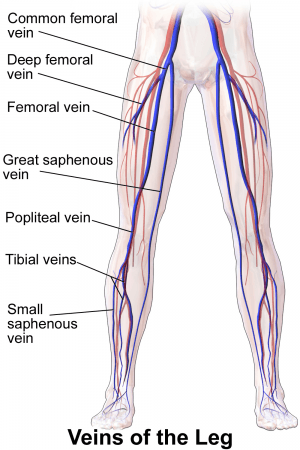
Significant risk of PE:
- Common femoral vein
- (Superficial) femoral vein
- (Superficial) femoral vein is part of the deep system, not the superficial system as the name suggests!
- Popliteal veins
Clinical Features


- Leg swelling with circumference >3cm more than unaffected side
- Tenderness over calf muscle
- Homan's sign - pain during dorsiflexion of foot (SN 60-96% and SP 20-72%)[3]
Differential Diagnosis
- Arterial thrombosis
- Arteritis
- Arthritis
- Buerger disease
- Cellulitis
- Compartment syndrome
- Complex regional pain syndrome
- Fracture
- Gout
- Lymphangitis
- Myositis
- Necrotizing fasciitis
- Nerve entrapment
- Neuropathy
- Osteomyelitis
- Paget-Schroetter syndrome
- Sciatica
- Septic Joint
- Tendonitis
Calf pain
Unilateral leg swelling
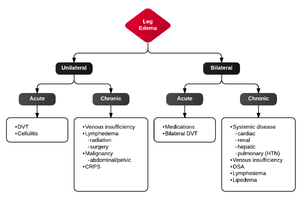
- Gravitational
- Venous insufufficiency
- Thrombophlebitis
- Lymphedema
- Medications
- Deep venous thrombosis (uncomplicated)
- Leg or foot infection
- Fracture
- Compartment syndrome
- Limb hypertrophy
- Hypertrophy of soft tissue or bone (Klippel-Trenaunay syndrome)
- Overgrowth of body part (Proteus Syndrome)
- Lipedema
- Tumor
- Post-thrombotic Syndrome
- Causes of bilateral pedal edema
Evaluation
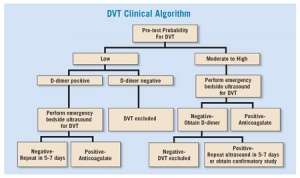
- Clinical exam
- Risk stratification for further testing indicated using, e.g. Modified Wells Score
Modified Wells Score
Can be applied for patients whose clinical presentation is concerning for a DVT in order to risk stratify.
- Active cancer (<6 mo) (1pt)
- Paralysis, paresis, or immobility of extremity (1pt)
- Bedridden >3 days because of symptoms within 4 weeks (1pt)
- TTP along deep venous system (1pt)
- Entire leg swollen (1pt)
- Unilateral calf swelling >3cm below tibial tuberosity (1pt)
- Unilateral pitting edema (1pt)
- Collateral superficial veins, not varicose (1pt)
- Previously documented DVT (1pt)
- Alternative diagnosis as likely or more likely than DVT (-2pts)
- A score of 0 or lower → minimal risk - DVT prevalence of 5%. D-dimer testing is safe in this group - negative d-dimer decreases the probability of disease to <1% allowing an ultrasound to be deferred.
- A score of 1-2 → moderate risk - DVT prevalence of 17%. D-dimer testing still effective and a negative test decreases post-test probability disease to <1%
- A score of 3 or higher → high risk - DVT prevalence of 17-53% → patients should receive an ultrasound[4]
Upper extremity DVT
Requires ultrasound for diagnosis. Cannot be ruled out with d-dimer.[5]
- Generally involves axillary or subclavian veins
- Primary upper extremity DVT typically presents in young healthy individuals
- Secondary upper extremity DVT often due to indwelling catheters
- Obtain a chest x-ray to rule out bony abnormalities that may be causing venous obstruction
Management
The distinction between distal and proximal relates to veins below and above the knee respectively.[6] Patients with superficial venous thromboses such as the long saphenous and short saphenous are at risk of developing a DVT, especially in patients who have a history of prior DVT although management with anticoagulation is controversial.[7]
Proximal DVT
Proximal veins are the external iliac, common femoral, greater saphenous, profound femoral, (superficial) femoral vein, popliteal vein
Distal DVT
Distal veins are the anterior tibial, posterior tibial, peroneal, gastrocnemius, soleus.
VTE in Pregnancy[8]
- Therapeutic LMWH or unfractionated heparin anticoagulation dose in:
- Antepartum outpatient with multiple prior VTEs or any VTE with high-risk thrombophilia until 6 weeks postpartum
- Postpartum inpatient with prior unprovoked, estrogen-provoked VTE, or low-risk thrombophilia for duration of admission
- Lower prophylactic anticoagulation dose in:
- Antepartum outpatient with prior unprovoked, estrogen-provoked VTE, or low-risk thrombophilia until6 weeks postpartum
- Patients admitted > 72 hrs, not at high risk for bleeding or imminent delivery
- Resume 12 hours after C-section and removal of epidural / spinal needle in indicated patients
- Halt anticoagulation if imminent delivery, C-section, epidural / spinal needle
Recurrent DVT on Therapeutic Anticoagulation
- Admit patients for vascular surgery and hematologist consult
- Consider Greenfield IVC filter placement
- Typically start heparin for additional anticoagulation
Upper extremity DVT
- If secondary to catheter, do not necessarily have to remove [9]
- Anticoagulation as per lower extremity DVTs.
- Patient should be admitted
Anticoagulation Options
| Medication | Warfarin (Coumadin) | Rivaroxaban (Xarelto) | Apixaban (Eliquis) |
| Standard Dosing |
|
|
|
| Renal Dosing |
|
|
|
Contraindications to anticoagulation
- Active hemorrhage
- Platelets <50
- History of intracerebral hemorrhage
Disposition
Discharge
Consider if all of the following are present:
- Ambulatory
- Hemodynamically stable
- Low risk of bleeding in patient
- Absence of renal failure
- Able to administer anticoagulation with appropriate monitoring
- Able to arrange for 2-3 day follow-up
Admit
For any of the following:
- Ileofemoral DVT that is a candidate for thrombectomy (should have the following):[10]
- Acute iliofemoral DVT (symptom duration <21 days)
- Low risk of bleeding
- Good functional status and reasonable life expectancy
- Phlegmasia cerulea dolens
- High risk of bleeding on anticoagulation
- Significant comorbidities
- Symptoms of concurrent PE
- Recent (within 2 weeks) stroke or transient ischemic attack
- Severe renal dysfunction (GFR < 30)
- History of heparin sensitivity or Heparin-Induced Thrombocytopenia
- Weight > 150kg
- Upper extremity DVT
See Also
External Links
References
- Righini M, Le GG, Aujesky D, et al. Diagnosis of pulmonary embolism by multidetector CT alone or combined with venous ultrasonography of the leg: a randomised non-inferiority trial. Lancet. 2008; 371(9621):1343-1352.
- Daniel KR, Jackson RE, Kline JA. Utility of the lower extremity venous ultrasound in the diagnosis and exclusion of pulmonary embolism in outpatients. Ann Emerg Med. 2000; 35(6):547-554.
- Anand SS, et al. Does this patient have deep vein thrombosis? JAMA. 1998; 279(14):1094-9.
- Del Rios M et al. Focus on: Emergency Ultrasound For Deep Vein Thrombosis. ACEP News. March 2009. https://www.acep.org/clinical---practice-management/focus-on--emergency-ultrasound-for-deep-vein-thrombosis/
- Kucher N. Clinical practice Deep-vein thrombosis of the upper extremities. N Engl J Med. 2011;364:861–869.
- Gualtiero P. How I treat isolated distal deep vein thrombosis (IDDVT). Blood 2014 123:1802-1809; doi: https://doi.org/10.1182/blood-2013-10-512616
- Litzendorf ME. Satiani B. Superficial Venous thrombosis:disease progression and evolving treatment approaches. Vasc Health Risk Manag. 2011(7). 569-575
- DʼAlton ME et al. National Partnership for Maternal Safety: Consensus bundle on venous thromboembolism. Obstet Gynecol 2016 Oct; 128:688.
- Kovacs MJ et al. A pilot study of central venous catheter survival in cancer patients using low-molecular-weight heparin (dalteparin) and warfarin without catheter removal for the treatment of upper extremity deep vein thrombosis (the catheter study) JTH. 2007;5:1650–1653.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4646749/