DVT ultrasound
Background
- Bedside ultrasound can be used to conduct compression testing on lower extremity vasculature to assess for DVT
- Intended to be rapid, limited, but revealing most clinically significant DVTs
- Amongst ED providers, there is a sensitivity of 95% and specificity of 96%[1]
Indications
- Clinical suspicion of DVT: edema, tenderness over the calf, Homan's sign
- Clinical suspicion of PE: chest pain, shortness of breath, tachycardia, tachypnea
Technique
Sites of Compression for 3-Point Evaluation
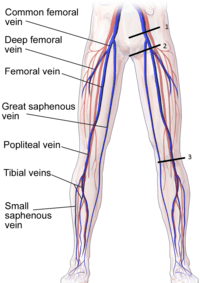
- Common Femoral Vein
- Saphenofemoral Junction
- Popliteal Vein
Steps
- Select transducer
- Linear array vascular probe 6–10 MHz
- For morbidly obese patients, consider abdominal probe
- Common Femoral Vein and Saphenofemoral Junction
- Patient positioning
- Reverse Trendelenburg or semi-sitting with 30 degrees of hip flexion
- Mild external rotation (30 degrees) hip
- Probe at medial inguinal crease
- Apply generous compression every centimeter
- Continue distal to 1-2cm beyond bifurcation of the common femoral vein
- Patient positioning
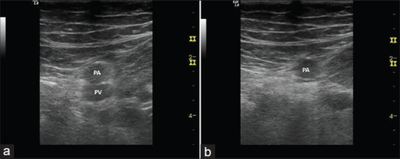
- Popliteal vein
- Patient positioning
- Prone, decubitus position, or seated on edge of gurney
- Knee flexed 10–30 degree
- Reverse Trendelenburg
- Start with light pressure to better visualize vessels
- Apply generous compression over the popliteal vessels to test compressibility
- Vein usually superficial to the artery (artery is anterior)
- Patient positioning
Findings
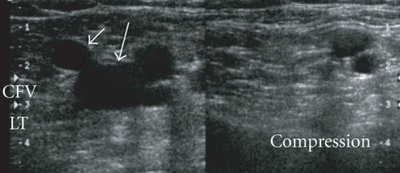
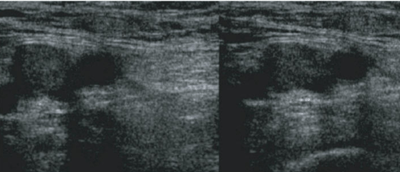
- Each segment of vein identified must be assess as compressible and noncompressible
- Touching of the anterior and posterior walls indicates a normal exam
- No touching with pressures sufficient to deform the artery indicates DVT
Images
Normal
Abnormal
Pearls and Pitfalls
- Arteries are the thick walled and more circular vessels identified
- Doppler flow can be used to identify different directions of flow in vessels and to identify no vascular structures
- Noncompressible vein may be mistaken for an artery, leading to a false negative result
- An artery may be mistaken for a non-compressible vein, leading to a false positive result
- Lymph nodes may be confused with noncompressible vein and if found, can be identified by moving up or down 1 cm
- Does not rule out calf DVTs
- For a more thorough exam, scan from the saphenofemoral junction down through the adductor canal in addition to the areas described above
- Use a curvilinear probe for obese or edematous patients
- An appropriate amount of pressure gives complete collapse of the vein as well as some (but not full) compression of the adjacent artery.[3]
Documentation
Normal Exam
A bedside ultrasound was conducted to assess for DVT with clinical indications of edema and pain. The extremity was assessed at 3 locations – common femoral vein, saphenofemoral junction, and the popliteal vein. Sequential compressions at these sites showed fully compressible veins. No sonographic evidence of DVT at these sites.
Abnormal Exam
A bedside ultrasound was conducted to assess for DVT with clinical indications of edema and pain. The extremity was assessed at 3 locations – common femoral vein, saphenofemoral junction, and the popliteal vein. Sequential compressions at these sites showed a noncompressible popliteal vein. DVT is present at the level of the popliteal vein.
Clips
Normal Study - No DVT
Abnormal Study - Incompressible left Common Femoral Vein
External Links
See Also
- Ultrasound (Main)
- Deep venous thrombosis
- Pulmonary embolism
- Paget-Schroetter syndrome
References
- Burnside P, Brown M, and Kline J. Systematic review of emergency physician-performed ultrasonography for lower-extremity deep vein thrombosis. Acad Emerg Med. 2008; 15:493–498.
- http://www.thepocusatlas.com/soft-tissue-vascular/
- Kline JA et al. Annals of Emerg Med, 2008. PMID: 18562044
- http://www.thepocusatlas.com/soft-tissue-vascular/
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.