Clostridium difficile (peds)
This page is for pediatric patients; for adult patients see clostridium difficile.
Background

Pseudomembranous colitis with yellow pseudomembranes seen on the wall of the sigmoid colon.
- Clostridium is a genus of Gram-positive bacteria
- Most common cause of infectious diarrhea in hospitalized patients
- Use contact isolation if suspect
- Alcohol-based hand sanitizers do not reduce spores, but good hand washing does[1]
Pediatric Risk Factors
- Antibiotic exposure, particularly penicillins, cephalosporins, clindamycin, fluoroquinolones
- PPIs
- GI feeding tubes
- Comorbidities - cancer, recent surgery, hospitalizations
Clinical Features
Varies according to severity and intrinsic host factors (immunosuppression, etc.).
- Diarrhea that develops during antibiotic use or within 2 weeks of discontinuation
- Usually occurs after 7-10 days of antibiotics, as diarrhea before that time is more often poor tolerance to antibiotic
- Recent discharge from hospital
- Profuse watery diarrhea
- Abdominal pain/tenderness
- Fever
- At the extreme, may present with sepsis secondary to intestinal perforation or toxic megacolon
Differential Diagnosis
Infectious
- Viral (e.g. rotavirus)
- Bacterial
- Campylobacter
- Shigella
- Salmonella (non-typhi)
- Escherichia coli
- E. coli 0157:H7
- Yersinia enterocolitica
- Vibrio cholerae
- Clostridium difficile
- Parasitic
- Toxin
Noninfectious
- GI Bleed
- Appendicitis
- Mesenteric Ischemia
- Diverticulitis
- Adrenal Crisis
- Thyroid Storm
- Toxicologic exposures
- Antibiotic or drug-associated
Watery Diarrhea
- Enterotoxigenic E. coli (most common cause of watery diarrhea)[2]
- Norovirus (often has prominent vomiting)
- Campylobacter
- Non-typhoidal Salmonella
- Enteroaggregative E. coli (EAEC)
- Enterotoxigenic Bacteroides fragilis
Evaluation
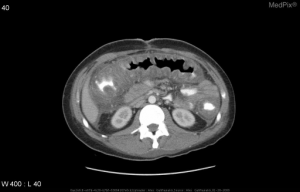
Pseudomembranous colitis from C. difficile on abdominal CT demonstratin diffuse colonic wall thickening and a shaggy endoluminal contour.
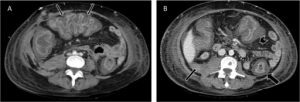
Pseudomembranous colitis with (A) Accordion sign in transverse colon (thin arrows). (B) Colonic wall thickness, target sign (thick arrow), peritoneal fluid (thin arrow) and pericolonic fat stranding (arrowhead).
Labs
- C. diff toxin assay
- Sn 63-94%, Sp 75-100%
- Culture
- Positive culture only means C. diff present, not necessarily that it is causing disease
Testing Algorithm
For patients with suspected Clostridium difficile associated diarrhea (CDAD)
- Low suspicion
- Send stool for C. diff toxin assay
- Positive → treat (no further testing indicated)
- Negative → do not treat (no further testing indicated)
- Send stool for C. diff toxin assay
- High suspicion
- Send stool for C. diff toxin assay AND treat empirically
- Positive → treat (no further testing indicated)
- Negative → Consider discussion with ID (false negative tests may occur); eval for other causes of diarrhea
- Send stool for C. diff toxin assay AND treat empirically
Repeat testing
- Never a need for repeat testing within 7 days of a previous test
- NO NEED to repeat positive tests as symptoms resolve as a “test of cure”
- NO NEED to repeat test soon after initial negative test (more likely to be a false positive test than a true positive test)
Management
- Stop offending antimicrobial agents, if possible
- Initial occurrence and first recurrence of mild-moderate disease:[5]
- PO metronidazole 30 mg/kg/d in four divided doses, max 2 g/day
- Severe infection or second recurrence:
- PO vancomycin 40 mg/kg/d in four divided doses, max 500 mg/day
- If no improvement after 24-48 hours, oral vancomycin max dose may be increased to 2 g/d
- Q6hr IV metronidazole, 30 mg/kg/d, may be added to intracolonic/enema vancomycin for ileus, inability to tolerate PO antibiotics
- 1-3 year old -- 250 mg vancomycin in 50 mL NS
- 4-9 year old -- 375 mg vancomycin in 75 mL NS
- > 9 year old -- 500 mg vancomycin in 100 mL NS
- Multiple recurrences, other strategies, in consult with pediatric GI:
- May benefit from tapering and pulse oral vancomycin over 1.5-2 months, as done in adults
- Consider PO fidaxomicin in ≥ 6 year old patients at 200 mg twice daily for 10 dats
Disposition
- Admit:
- Severe diarrhea
- Outpatient antibiotic failure
- Systemic response (fever, leukocytosis, severe abdominal pain)
Antibiotic Sensitivities[6]
See Also
References
- Leffler DA and Lamont JT. Clostridium difficile Infection. N Engl J Med. 2015; 372:1539-1548.
- Marx et al. “Cholera and Gastroenteritis caused by Noncholera Vibrio Species”. Rosen’s Emergency Medicine 8th edition vol 1 pg 1245-1246.
- Asymptomatic colonization by Clostridium difficile in infants: implications for disease in later life. Jangi S, Lamont JT. J Pediatr Gastroenterol Nutr. 2010 Jul; 51(1):2-7.
- Clostridium difficile Infection in children. Sammons JS, Toltzis P, Zaoutis TE. JAMA Pediatr. 2013 Jun; 167(6):567-73.
- D'Ostroph AR and So TY. Treatment of pediatric Clostridium difficile infection: a review on treatment efficacy and economic value. Infect Drug Resist. 2017; 10: 365–375.
- Sanford Guide to Antimicrobial Therapy 2014
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.