Esophageal perforation
Background
- Full thickness perforation of the esophagus
- Secondary to sudden increase in esophageal pressure
- Perforation is usually posterolateral
Causes
- Iatrogenic (most common)
- Endoscopy
- Boerhaave syndrome
- Thoracic Trauma
- Penetrating
- Blunt (rare)
- Caustic ingestion
- Foreign body
- Bone
- Button battery
- Infection (rare)
- Tumor
- Aortic pathology
- Barrett esophagus
- Zollinger-Ellison syndrome
Clinical Features
Mackler’s triad
- Pathognomonic for Boerhaave syndrome
- Chest pain
- Vomiting
- Subcutaneous emphysema
History
Physical Exam
- Cervical subcutaneous emphysema
- Mediastinal emphysema
- Takes time to develop
- Absence does not rule out perforation
- Hamman's sign
- Mediastinal crunching sound
- May rapidly develop sepsis due to mediastinitis
Differential Diagnosis
Critical
- Acute Coronary Syndromes
- Aortic dissection
- Cardiac tamponade
- Pulmonary embolism
- Tension pneumothorax
- Esophageal perforation (Boerhhaave's syndrome)
- Coronary artery dissection
Emergent
- Pericarditis
- Myocarditis
- Pneumothorax
- Mediastinitis
- Cholecystitis
- Pancreatitis
- Cocaine-associated chest pain
- Myocardial rupture
Nonemergent
- Stable angina
- Asthma exacerbation
- Valvular Heart Disease
- Aortic Stenosis
- Mitral valve prolapse
- Hypertrophic cardiomyopathy
- Pneumonia
- Pleuritis
- Tumor
- Pneumomediastinum
- Esophageal Spasm
- Gastroesophageal Reflux Disease (GERD)
- Peptic Ulcer Disease
- Biliary Colic
- Muscle sprain
- Rib Fracture
- Arthritis
- Costochondritis
- Spinal Root Compression
- Thoracic outlet syndrome
- Herpes Zoster / Postherpetic Neuralgia
- Psychologic / Somatic Chest Pain
- Hyperventilation
- Panic attack
Thoracic Trauma
- Airway/Pulmonary
- Cardiac/Vascular
- Cardiac injury
- Blunt cardiac injury
- Penetrating cardiac injury
- Cardiac tamponade
- Traumatic aortic transection
- Cardiac injury
- Musculoskeletal
- Other
Evaluation
Imaging[1]
- CXR: 90% will have radiographic abnormalities, nonspecific in nature
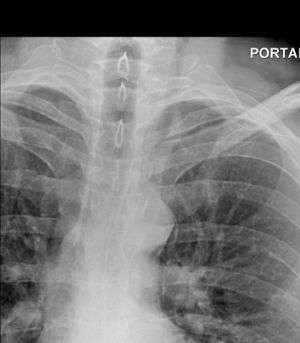
Mediastinal air adjacent to the aorta and tracking cephalad adjacent to the left common carotid artery.
- Pneumomediastinum
- Abnormal cardiomediastinal contour
- Pneumothorax
- Pleural effusion
- Esophagram
- Water soluble contrast
- Preferred study as it allows for definitive diagnosis
- CT chest
- May show pneumomediastinum
- Will not definitively show perforation
- Emergent endoscopy
- May worsen the tear during insufflation
Management
- Volume resuscitation
- Broad-spectrum IV antibiotics
- Emergent surgical consultation
Disposition
- Admit (generally to OR for emergent repair)
See Also
References
- Hess JM, Lowell MJ: Esophagus, Stomach and Duodenum, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 7. St. Louis, Mosby, Inc., 2010, (Ch) 89: p 1170-1187
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.