Atopic dermatitis
Background
- Also known as atopic eczema
- A chronic type of inflammatory skin disease affecting many children and adults
- Occasionally accompanied by asthma and/or hay fever. Patients develop a cutaneous hyperreactivity to environmental triggers.
- Cause is not known, but believed to be due to an interaction between susceptibility genes, the environment, defective skin barrier function, and immunologic responses.
Clinical Features
- Atopic personal or family history, worse in winter, dry weather
- Erythema, crusts, fissures, pruritus, excoriations, lichenification
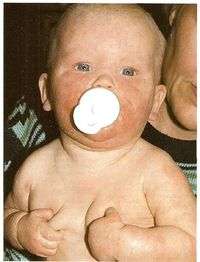
Infantile
- blisters, crusts, exfoliations
- Face, scalp, extremities, sparing of diaper area
- 1st few months of life, resolving by age 2
- Differentiate from impetigo (which may occur alongside)
Adults
- Dryness, thickening in flexor surfaces including antecubital and popliteal fossae, neck
Differential Diagnosis
Neonatal Rashes
- Atopic dermatitis
- Diaper dermatitis
- Erythema toxicum neonatorum
- Neonatal acne
- Psoriasis
- Seborrheic dermatitis
- Tinea capitis
- Impetigo
- Contact dermatitis
- Perianal streptococcal dermatitis
- Milia
- Miliaria
- Mongolian spots
- Omphalitis
- Pustular melanosis
- Sucking blisters
Evaluation
- Clinical diagnosis
- Dry skin, erythematous papular lesions
- Face most commonly involved; nose and diaper areas spared
Neonatal atopic dermatitis vs. seborrhoeic dermatitis
| Category | Neonatal atopic dermatitis | Neonatal seborrhoeic dermatitis |
| Presentation | 1-2 months | 2-6 months |
| Puritic (fussiness) | Yes | No |
Management
- Identify and eliminate triggers:
- Alcohol based products
- Fragrances and astringents
- Excessive bathing
- Allergens
- Reduce drying of skin
- Avoid lotions (high water and low oil content)
- Liberal application of emollients (vaseline) immediately after bath (<5 min, skin should be pat dry instead of rubbing) [1]
- Alternatives include petroleum jelly and Aquaphor
- If using steroids, apply emollients on top of steroids
- Topical steroids
- 7 days of low or medium potency steroid ointments either daily or BID
- Triamcinolone, hydrocortisone, or betamethasone
- Severe flares require high potency steroids followed by a taper
- Topical steroid potency for additional options
- 7 days of low or medium potency steroid ointments either daily or BID
- Avoid fluoridinated steroids to thin skin areas such as face, groin, or axilla
- Consider doxepin for recalcitrant pruritus[2][3]
- 25-50mg PO nightly
- Or topical doxepin cream 5% QID
Disposition
- Outpatient
Complications
- Secondary bacterial infection
- Eczema herpeticum, widespread HSV infection
- Dyshidrotic eczema
References
- Fang J. Dermatology. In: The Harriet Lane Handbook. 20th ed. Philadelphia, PA: Elsevier; 2015
- Hercogova J. Topical anti-itch therapy. Dermatol Ther 18(4):341-3 (2005 Jul-Aug).
- Drake L, Cohen L, Gillies R, et al. Pharmakinetics of doxepin in subjects with pruritic atopic dermatitis. J Am Acad Dermatol 41(2):209-14 (1999 Aug).
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.