Anthrax
Background
- Gram positive rod, Bacillus anthracis, which is capable of surviving inhospitable condition through the formation of endospores. tough spores
- Incubation period is 10 days with no ability for human to human transmission and therefore, no need for respiratory isolation
- Though human to human transmission does not occur, potential harbors of spores (patient clothes) need to be isolated and decontaminated with 10% bleach[1]
- In general there is cutaneous, inhalational, and gastrointesinal anthrax.
Inhalational (5%)
- Biphasic course
Prodrome Period
- Early prodromal period often appears as an flu-like illness
- Fever, dry cough, myalgia, malaise
- Transient clinical improvement followed by rapid decline
Acute phase
- Severe respiratory distress with symptoms consisting of[2]:
- Hypoxia, tachypnea, cyanosis
- Severe dyspnea, chest pain
- Shock
- Mediastinitis
Cutaneous (95%)
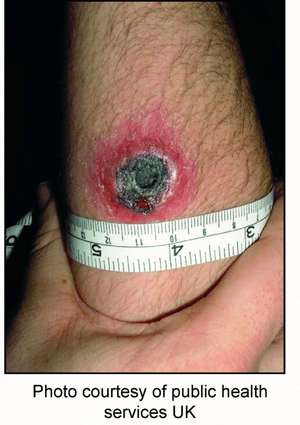
Cutaneous anthrax
- The disease will start as an area of erythema and edema and progress to a vesicle which ruptures forming a central black eschar
- Total course of lesion evolution occurs over 1 week
Gastrointestinal
- Over the course of 7 days, nonspecific abdominal pain, nausea and vomiting with progress to severe abdominal pain, bloody emesis and diarrhea (usually bloody)[3]
Differential Diagnosis
Cutaneous (painless)
- Ecthyma gangrenosum
- Rat-bite fever (Streptobacillus monilifomis and Spirillum minus)
- Ulceroglandular tularemia
- Plague
- Glanders (Pseudomonas peudomallei)
- Rickettsial pox (Rickettsia akari)
- Orf (parapox virus)
- Staph lymphadenitis
- TB
- Leprosy
- Buruli ulcer (Mycobact ulcerans)
Inhalational
- Acute bacterial mediastinitis
- Mycoplasma
- Legionnaire's
- Psittacosis
- Tularemia
- Q fever (Coxiella burnetti)
- Viral pneumonia
- Histoplasmosis
- Coccidiomycosis
- Ruptured Aortic Dissection
- SVC syndrome
- Silicosis
- Sarcoidosis
Lower Respiratory Zoonotic Infections
- Psittacosis
- Anthrax (Bacillus anthracis)
- Brucellosis (Brucella species)
- Q fever (C. burnetti)
- Pasteurellosis (Pasteurella multocida)
- Melioidosis (Burkholderia pseudomallei)
- Rocky Mountain Spotted Fever (R. rickettsii)
- Pulmonic Plague (Yersinia pestis)
- Influenza A
- Hantavirus
Bioterrorism Agents[4]
Category B
- Ricin
- Brucellosis
- Epsilon toxin
- Psittacosis
- Q Fever
- Staph enterotoxin B
- Typhus
- Glanders
- Melioidosis
- Food safety threats
- Water safety threats
- Viral encephalitis
Evaluation
- CXR/CT
- Widened mediastinum representing hemorrhagic mediastinitis
- Infiltrate, pleural effusion
- Hyperdense mediastinal lymphadenopathy
Management
Contact CDC Emergency Hotline 1-707-488-7100 for all suspected bioterrorism cases
Postexposure Prophylaxis
Patient should be vaccinated at day #0, #14, #28
- Ciprofloxacin 500mg PO q12hrs daily x 60 days OR
- Doxycycline 100mg PO q12hrs x 60 days
Cutaneous Anthrax (not systemically ill)
- Ciprofloxacin 500mg PO q12hrs x 60 days
- Doxycycline 100mg PO q12hrs x 60 days
Inhalation or Cutaneous with systemic illness
- Ciprofloxacin 400mg IV q12hrs x 60 days (1st line) OR
- Doxycycline 100mg IV q12hrs x 60days (only if allergic to ciprofloxacin) PLUS
- Clindamycin 900mg IV q8hrs
Pediatric Postexpsoure Prophylaxis
- Ciprofloxacin 15mg/kg PO q12hrs x 60 days
- Doxycycline 2.2mg/kg PO q12hrs x 60 days
Pediatric Cutaneous Anthrax (not ill)
- Same as post exposure dosing and duration
Pediatric Inhalational or Cutaneous (systemically ill
- Ciprofloxacin 15mg/kg IV q12hrs (1st line) OR
- Doxycycline 2.2mg/kg IV q12hrs (only if allergic to cipro) PLUS
- Clindamycin 7.5mg/kg q6hrs daily
Disposition
- Admit
See Also
References
- Heninger SJ et al. Decontamination of Bacillus anthracis Spores: Evaluation of Various Disinfectants. Appl Biosaf. 2009 Jan 1; 14(1): 7–10.
- Medscape: Anthrax
- CDC. Gastrointestinal anthrax after an animal-hide drumming event - New Hampshire and Massachusetts, 2009. MMWR Morb Mortal Wkly Rep. 2010 Jul 23;59(28):872-7. http://www.ncbi.nlm.nih.gov/pubmed/20651643
- https://www.niaid.nih.gov/topics/biodefenserelated/biodefense/pages/cata.aspx Accessed 02/26/16
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.