Acute mountain sickness
Background
- Also referred to as AMS
- Usually only occurs with altitude >7,000-8,000ft
- May occur at lower altitudes in patients who are particularly susceptible (COPD, CHF)
- Development of symptoms based on: rate of ascent, sleeping altitude, strength of hypoxic ventilatory response, alcohol intake, obesity
- NOT based on physical fitness, age, sex, smoking, previous high-altitude experience
- Tend to have recurrence of symptoms whenever they return to the symptomatic altitude
Clinical Features
- Clinical diagnosis with recent ascent to high altitude (usually >2000m)
- Requires headache + 1 or more of the following:[1]
- Ataxia and confusion heralds onset of headache
- Periodic breathing, particularly during sleep
Onset
- Symptoms usually develop 1-6hr after arrival at elevation
- May be delayed for 1-2d
- Especially common after the 1st or 2nd night's sleep
Duration
- Average duration of symptoms at 10,000ft = 15hr
- At higher elevations symptoms may last weeks / more likely to progress to headache
Differential Diagnosis
- Dehydration
- AMS is not improved by fluid administration alone
- Body hydration does not influence susceptibility to AMS
- Exhaustion
- Viral syndrome
- Alcohol hangover
- Caffeine withdrawal
- Hypothermia
- CO poisoning
- CNS infection: Meningitis, Encephalitis
- Cerebral venous sinus thrombosis
- Migraine
- Whereas supplemental O2 helps headache due to AMS in 10-15min, O2 has no effect on migraines
- TIA
- Hypoglycemia
Evaluation
- Clinical diagnosis
- Mental status, cerebellar exam - rule out HACE
- Lung exam - rule out HAPE
- Lake Louise Scoring System: Sum of symptoms 0-3 (none, mild, moderate, severe/incapacitating). Mild corresponds to score 3-4, Moderate-severe corresponds to score ≥5
- Headache
- Gastrointestinal symptoms
- Fatigue/weakness
- Lightheadedness
- Difficulty Sleeping
Management
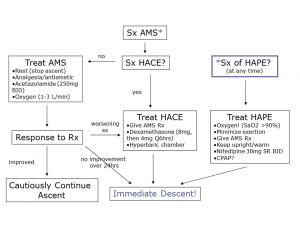
High altitude management algorithm.
Mild
- Terminate ascent and/or descend [3]
- Descend to lower altitude (by 1000-3000ft) OR acclimatize for 12-36hr at same altitude
- Acetazolamide
- Mechanism: speeds acclimatization by promoting bicarb diuresis
- Indications:
- History of altitude illness
- Abrupt ascent to >9800ft
- AMS requiring treatment
- Bothersome periodic breathing during sleep
- 125-250mg PO BID until symptoms resolve
- Side-effects
- Allergic reaction (if patient allergic to sulfa), paresthesias, polyuria, carbonated beverages taste bitter
- Can also worsen dehydration by promoting bicarb diuresis
- Symptomatic treatment as necessary with analgesics (NSAIDs) and antiemetics (ondansetron)
- Sleep-agents
- Benzos are only safe if given in conjunction with acetazolamide
- Nonbenzodiazepines are safe (zolpidem, diphenhydramine)
Moderate-Severe
- Immediate descent for worsening symptoms
- Low-flow 0.5-1 L/min O2 if available (especially nocturnal administration)
- Acetazolamide 250mg PO BID
- Dexamethasone 4mg PO q6hr
- Symptom-improvement only; unlike acetazolamide does not aid acclimatization
- Hyperbaric therapy
Prevention
- Graded ascent with adequate time for acclimatization is the best prevention
- Acetazolamide prophylaxis
- Indicated for patients with history of altitude illness or forced rapid ascent to altitude
- Start 24hr before ascent and continue for the first 48hrs at peak altitude
- Can be restarted if illness develops
- Reduces symptoms of AMS by 75% in patients ascending rapidly to altitudes >8200ft
- Dexamethasone[4]
- Start day of ascent and continue for first 2 days at altitude
- 4mg PO q12hr
- Prevents and treats cerebral edema
- Ginkgo biloba
- Controversial if effective; safe
- Ibuprofen
- Prevention - less effective than acetazolamide, better than placebo
- Treatment of headache (however, important to consider that taking ibuprofen may mask symptoms)
Disposition
See Also
References
- Schneider M et al. Acute mountain sickness: Influence of susceptibility, preexposure, and ascent rate. Med Sci Sports Exerc 2002; 34:1886-1891.
- Gallagher, MD, Scott A.; Hackett, MD, Peter (August 28, 2018). "High altitude pulmonary edema". UpToDate. Retrieved May 2, 2019.
- Luks A, McIntosh S, Grissom C, Auerbach P, Rodway G, Schoene R, Zafren K, Hackett P. Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2014 Update. Wilderness Environ Med. 2014; S4-S14.
- Luks AM, McIntosh SE, Grissom CK, et al. Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Acute Altitude Illness: 2014 Update. Wilderness & Environmental Medicine. 2014(25): S4–S14)
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.