Abscess
Clinical Features
- Tender nodular region with surrounding induration
- Fluctuance
- Surrounding erythema
Differential Diagnosis
- Cyst
- Vascular malformation
Skin and Soft Tissue Infection
- Cellulitis
- Erysipelas
- Lymphangitis
- Folliculitis
- Abscess
- Necrotizing soft tissue infections
- Mycobacterium marinum
Evaluation

Fluctulance on exam
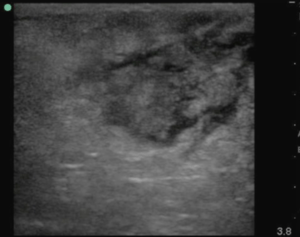
Abscess on ultrasound
- Clinical exam: fluctulance +/- erythema
- Soft tissue ultrasound can differentiate between abscess and cellulitis
- Assess for fluid collection and swirl within the collection
- Recent small studies have shown limited utility to bedside ultrasound in this capacity as it rarely leads to change in management (i.e. when a provider feels there is an abscess present, ultrasound shows an abscess and when there is diagnostic uncertainty the ultrasound usually is unequivocal as well)[4]
Management
- Incision and drainage
- Packing
- Abscess >5 cm in diameter
- Pilonidal abscess
- Abscess in an immunocompromised or diabetic patient
- Alternative to packing is loop drainage technique with vessel ties[5] or cut the proximal cuff of the sterile gloves[6]
- Failure rate of 4.1% for loop vessel technique vs 9.8% for conventional packing. [7]
- Other advantage is don’t have to keep coming back to the ER for painful repacking.
- Home Care (copied from Pediatric EM Morsels)[8]
- Keep area clean.
- Can cover with gauze to absorb the residual drainage.
- Can shower and/or bathe.
- The loop drain can be removed when (copied from Pediatric EM Morsels)[9]
- Drainage has stopped.
- Cellulitis has improved.
- Usually is within 7-10 days.
- Antibiotics
- Although withholding antibiotics is part of Choosing wisely ACEP, new evidence suggest antibiotic NNT of 14 to prevent 1 treatment failure[10]
- TMP/SMX DS BID x 5 days (all abscesses)[11]
- Consider more aggressive antibiotic treatment if concomitant cellulitis
Disposition
Admission
- Reserved for significantly ill patients or those requiring surgical intervention
Discharge
- Appropriate for majority of patients
- Follow up in 2 days for wound check
External Links
References
- Maligner D et al. The prevalence of community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) in skin abscesses presenting to the pediatric emergency department. N C Med J. 2008 Sep-Oct;69(5):351-4.
- Pickett A et al. Changing incidence of methicillin-resistant staphylococcus aureus skin abscesses in a pediatric emergency department. Pediatr Emerg Care. 2009 Dec;25(12):831-4.
- Bradley W. Frazee et al. High Prevalence of Methicillin-Resistant Staphylococcus aureus in Emergency Department Skin and Soft Tissue Infections http://dx.doi.org/10.1016/j.annemergmed.2004.10.011
- Effect of initial bedside ultrasonography on emergency department skin and soft tissue infection management Mower WR, Crisp JG, Krishnadasan A, et al. Ann Emerg Med. 2019;74(3):372-380.
- Incision and Loop Drainage of Abscess BY SEAN M. FOX Pediatric EM Morsels
- Sterile Glove Used As a Drain for a Skin Abscess? SinaiEM
- Am J Emerg Med, 2018. Comparison of the loop technique with incision and drainage for soft tissue abscesses: A systematic review and meta-analysis.
- Incision and Loop Drainage of Abscess BY SEAN M. FOX Pediatric EM Morsels
- Incision and Loop Drainage of Abscess BY SEAN M. FOX Pediatric EM Morsels
- Talan DA, et al. Trimethoprim–Sulfamethoxazole versus placebo for uncomplicated skin abscess. NEJM. 2016; 374(9):823-832.
- EBQ:TMP-SMX vs Placebo for Uncomplicated Skin Abscess
This article is issued from
Wikem.
The text is licensed under Creative
Commons - Attribution - Sharealike.
Additional terms may apply for the media files.